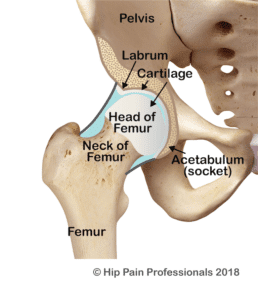
Acetabular dysplasia refers to an underdeveloped hip socket, or, the “acetabulum” the underdevelopment either affecting the bones, or the alignment/orientation of the socket or both. This bony problem, may in some people, result in increased movement (shearing) in hip joint resulting in instability (and in some cases dislocation) of the joint. Early wear of the joint structures and ultimately hip pain and osteoarthritis¹ can eventuate.
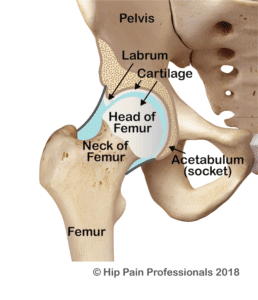
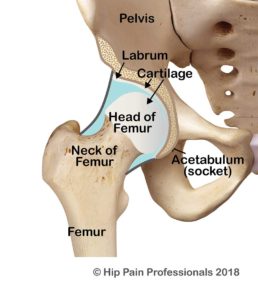
The hip socket is like a hemispherical cup that sits in the side of the pelvis. The opening of the cup faces out to the side and is normally tilted a little downwards and forwards. This provides a balance of joint mobility (flexibility) and stability. The socket and the ball (head of the femur) are normally of a similar shape and diameter, so that the socket hugs firmly around the ball (Figure 1). This allows the ball to swivel nicely around a centre point but controls excessive translation (sideways or back-forward motion). Optimal health of joint structures such as the cartilage (tissue that covers and protects the ends of long bones at the joints) and labrum (a triangular fibrocartilaginous fringe that joins the edge of the hip socket important for hip joint health) appear to be more easily maintained with this bony relationship between the ball and socket, that is, position, size and shape of the joints (outlined above) that allow for best mobility and stability.