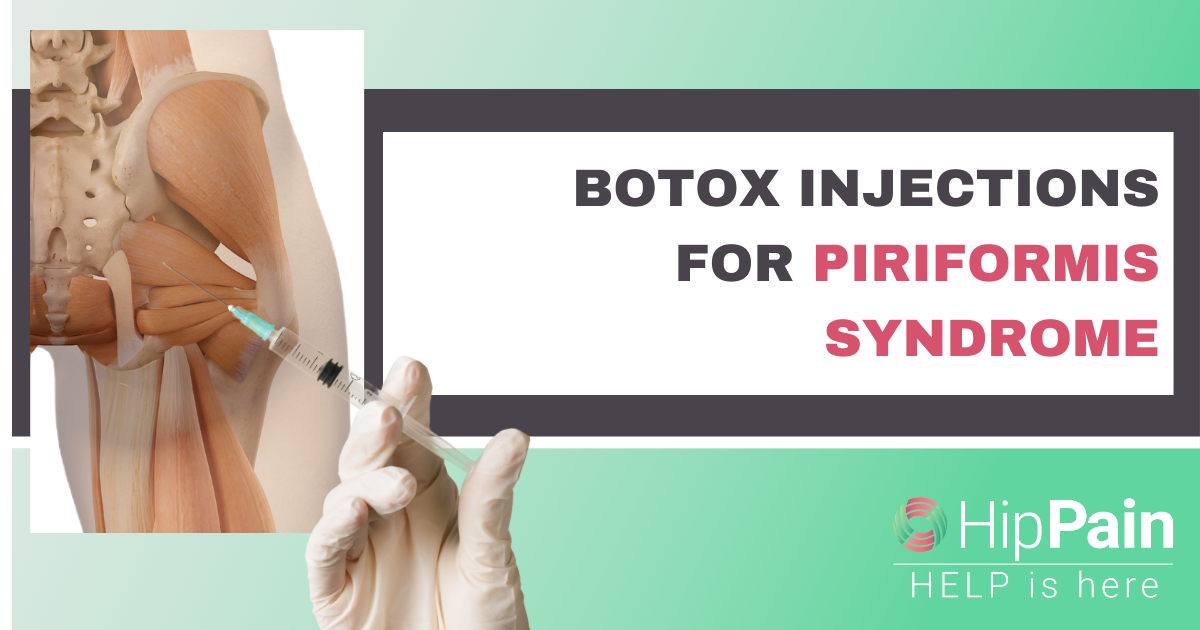
The sciatic nerve can sometimes be compressed, irritated or entrapped as it runs through the soft tissues of the buttock.
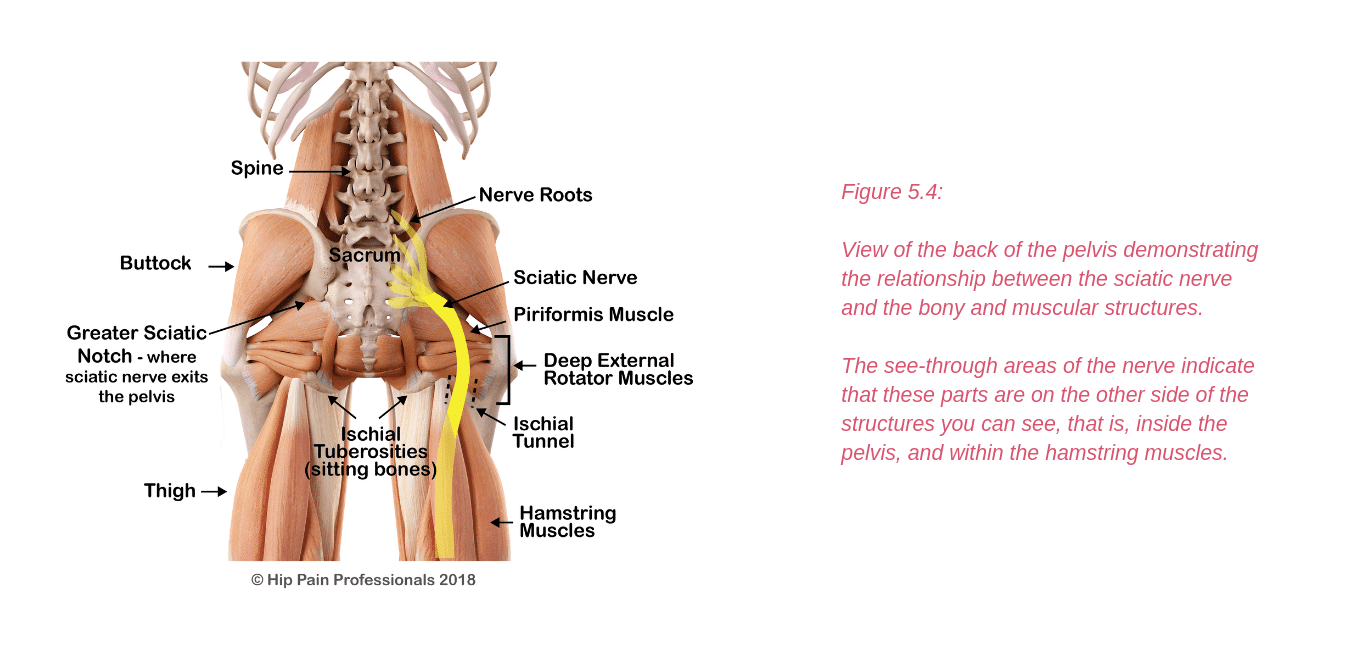
Traditionally, sciatic pain (neuralgia) generated from issues within the buttock has been termed “Piriformis Syndrome” (see Figure5.4 to view the piriformis muscle and the sciatic nerve).
This was based on a finding that in about 20% of the population, all or part of the sciatic nerve runst hrough the piriformis muscle. Compression of the nerve within the piriformis muscle was thought to be the problem in all cases of nerve-related buttock and leg pain that could not be associated with a problem in the back.
It is now thought that this is the case in only a relatively small number of cases and that this condition has been over-diagnosed. So much so, that some believe it does not exist at all.
The term “Deep Gluteal Syndrome” has been suggested recently as an alternative term to piriformis syndrome. It refers to any irritation of the sciatic nerve in the deep gluteal space, beneath the gluteus maximus muscle.
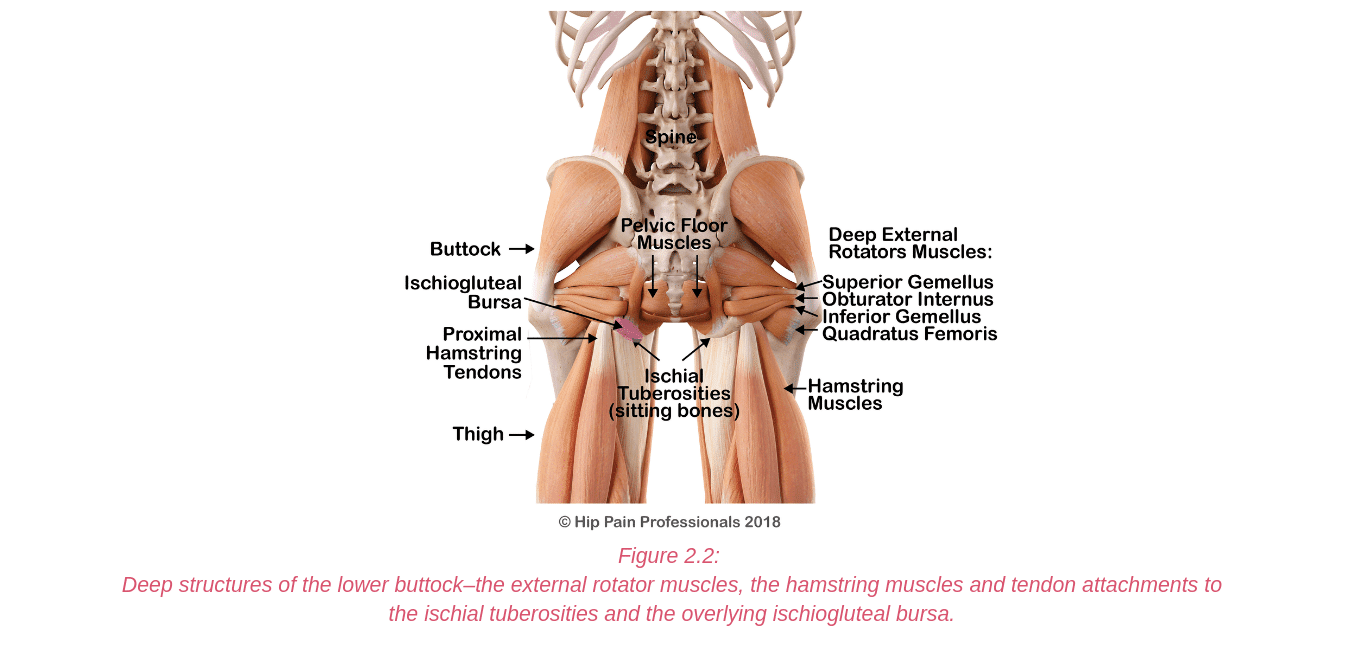
In this space, the sciatic nerve may be compressed or irritated at the level of the piriformis, as it runs over the deep external rotator muscles or by fibrous bands anywhere along its path through the buttock.
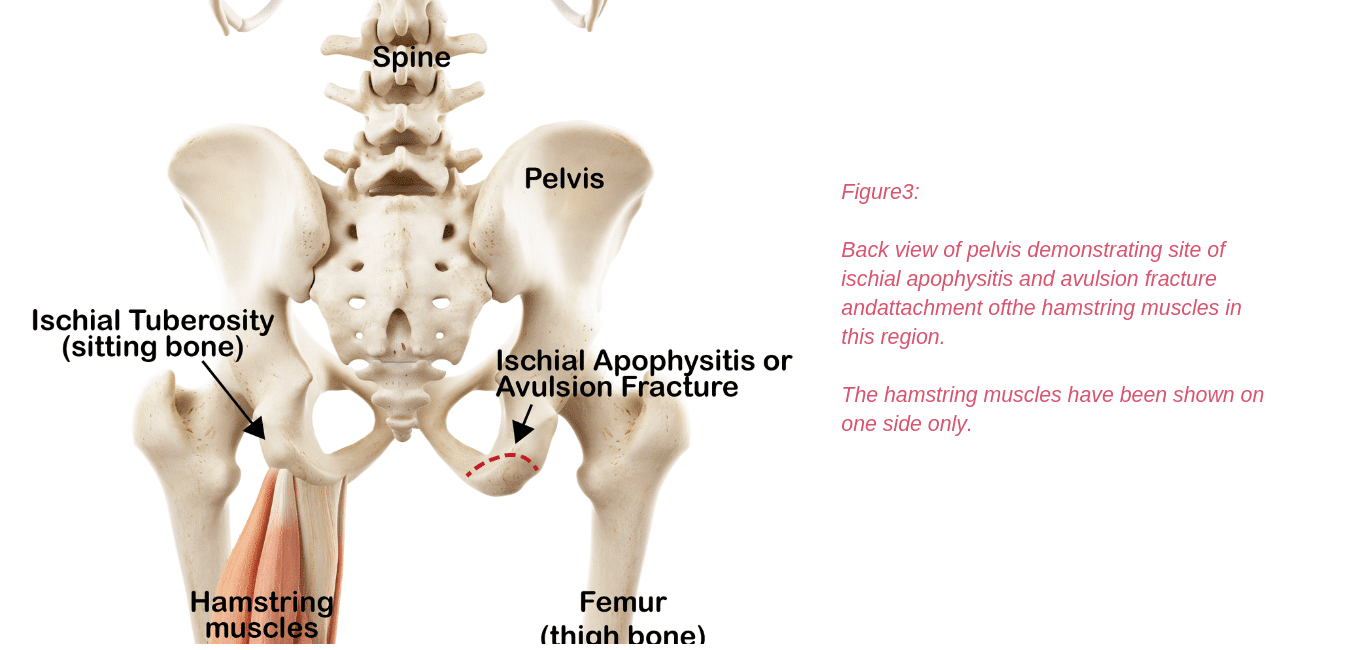
The nerve can also be irritated as it leaves the pelvis to head down into the thigh. Here it runs through a tunnel (ischial tunnel), between the outer side of the sitting bone (ischial tuberosity) and the upper thighbone (femur) (Figure5.4).
In this tunnel it may be squeezed between the bones or irritated by unhealthy hamstring tendons (tendinopathy).
Cluneal Nerve Neuralgia
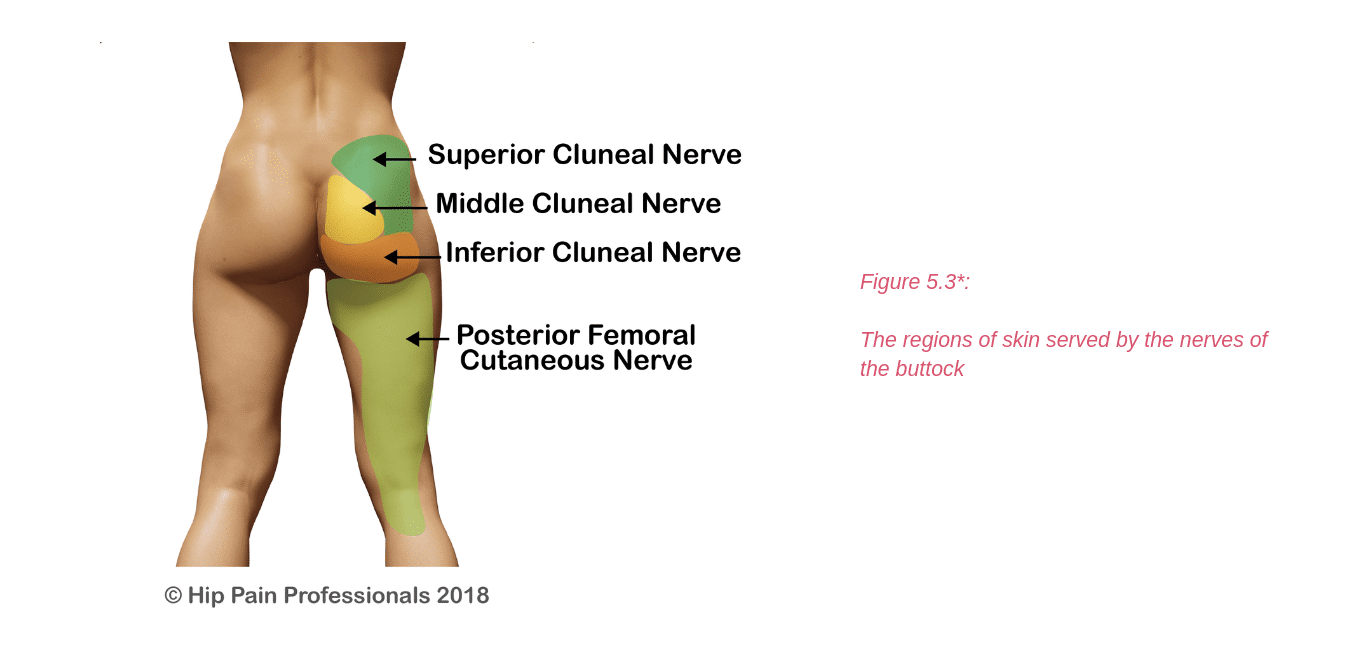
Of the cluneal nerves, the superior and inferior are more likely to be at risk of compression. Irritation of the superior cluneal nerve may result in upper buttock pain. The superior cluneal nerve branches run from the spine, over the top of the back of the pelvis and down into the buttock.
They usually run through fibrous tunnels as they cross the top edge of the pelvis. This is where the small nerves may become compressed or irritated. This is usually associated with a fairly localised area of pain in the upper buttock, in the region of its skin supply (Figure5.3).
Gluteal Nerve Neuralgia
The gluteal nerves do not have a sensory supply to the skin, but gluteal neuralgia may be felt as a deep buttock pain, sometimes like a cramping feeling.
These nerves provide important motor supply (the ability to make the muscles work/contract) to the gluteal muscles and the Tensor Fascia Lata (TFL) muscle at the side of the hip.
Damage to these nerves may alter your ability to stand on one leg, walk without a limp, climb stairs, and lift the leg out to the side or behind you. The nerves may be irritated or compressed as they pass out into the back of the pelvis and run through the soft tissues of the buttock.
Very occasionally, these nerves may also be damaged by surgery, such as a posterior approach Total Hip Replacement (where the scar is at the back of the hip).
For Pain Related to Nerves/Neuralgia throughout the Hip, Pelvis, Buttock and Groin:
- perform specific tests in the clinic to see if nerve involvement is likely
- provide treatments and give you exercises that may improve the health or movement of the nerve
- help improve health of the muscles and tendons beside the nerve (this may be the source of nerve irritation)
- review the positions you spend time in and activities you perform daily and provide strategies when performing these tasks that might help protect the nerve, thus reducing your symptoms. This may include changing your sitting or lying posture, or changing stretches or strength exercises that you have been performing that may be contributing to the irritation the nerve
- provide nerve gliding or mobility exercises that can be useful in some situations
- refer you for further tests or to a neurologist, orthopaedic specialist or other pain specialist if required
- In some cases, your hip pain professional may refer you to a pelvic floor physio for further assessment should they consider the pelvic floor muscles are involved
*Please note: Nerve supply can overlap and be quite variable between individuals. The diagrams provided in this section only provide an approximate guide of nerve supply in each region.


 Joint Related
Joint Related  Soft Tissue Related
Soft Tissue Related  Bone Related
Bone Related  Back Related
Back Related  Peripheral Nerve
Peripheral Nerve  Other causes
Other causes