Bone Related Pain
Although relatively more rare than soft tissue or joint problems, bony problems such as a fracture, stress fracture or very rarely, infection or tumour within the bone may cause hip and pelvic pain. In growing children or adolescents, pain may be related to disorders of the growth plates of the femurs or pelvis.
Bone Related Pain in the Front of the Hip
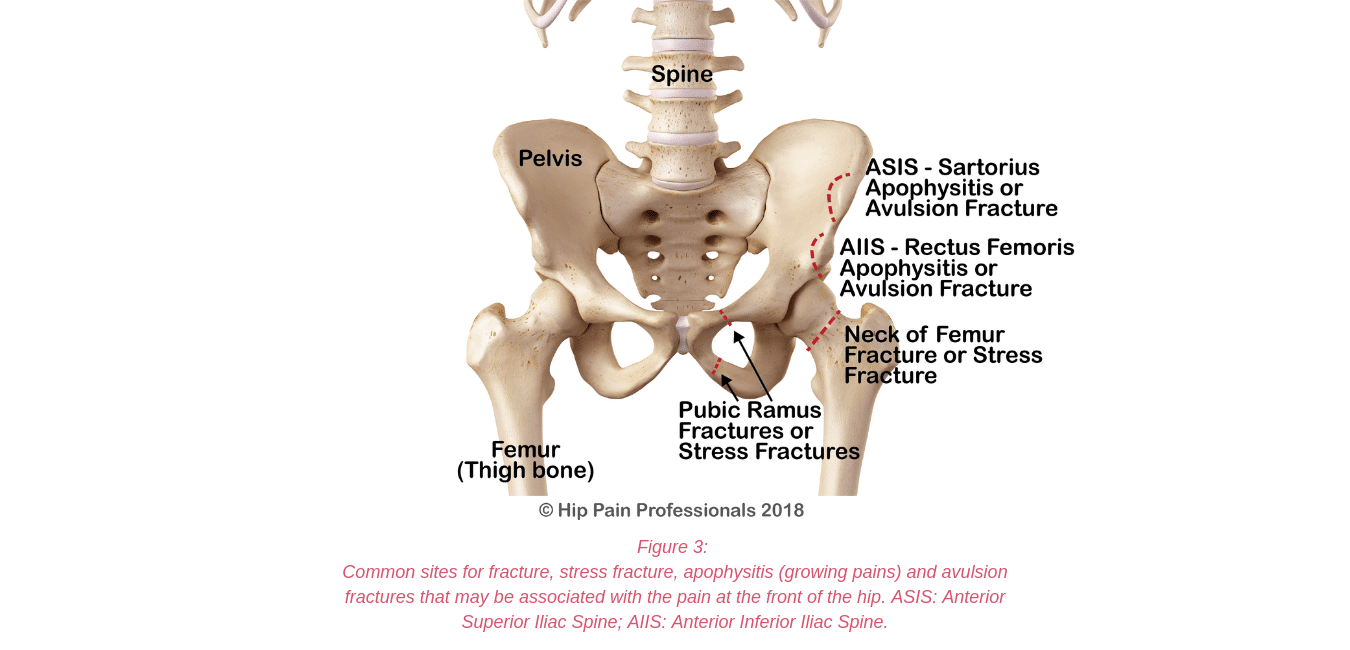
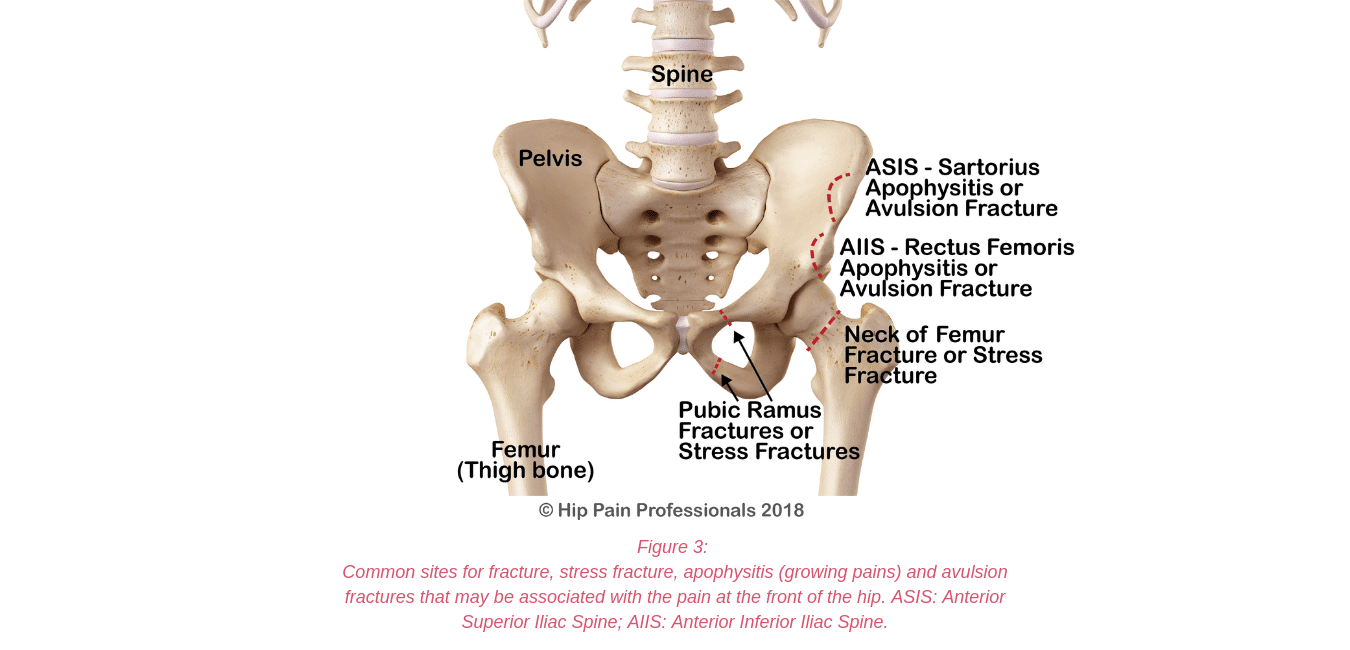
The most likely bone-related issues associated with pain in the anterior hip region, are fractures or stress fractures of the femur or pelvis (pubic ramus), or apophysitis or avulsion fracture of the growth plates at the front of the pelvis (ASIS & AIIS) (Figure 3).
Bone related pain may be due to:
- Fracture
- Stress fracture
- Avulsion fracture
- Apophysitis
A fracture:
- is the medical term for a broken bone
- usually occurs from a traumatic event like a fall, car accident or more severe sporting injury
- is more likely to occur in a weakened bone e.g. osteoporosis or genetic diseases like osteogenesis imperfecta
The most common fractures associated with anterior hip pain include a fracture of the neck of the femur (common in older women with osteoporosis) or fractures through the pelvis or the main shaft of the femur related to large trauma.
A stress fracture:
- is the medical term used for a fracture that occurs due to a build-up of repetitive stress
- is usually related to overuse -an accumulation of repeated small traumas e.g. long-distance running
- is more likely to occur with rapid increases in athletic training volume and/or inadequate recovery time
- starts as localised swelling in the area of bone exposed to highest stress (you won’t see this at skin level as it is just within the bone)–this may be called a stress reaction or bony stress response
- may progress to full fracture if you don’t rest
An avulsion fracture:
- is where a small piece of bone is pulled away from the main part of the bone
- may occur in adults where a large force across a ligament (joins bone – bone) or tendon (joins muscle to bone), causes a small piece of bone to come away with the ligament or tendon
- may occur in children at the bony growth plates (read more in the next section)
Apophysitis:
- usually referred to as ‘growing pains’
- occurs in adolescents
- is due to long bones such as the femur growing more quickly than the muscles, which then tug on the growth zones in the immature pelvis
- most commonly occurs at sites where some of the large muscles attach at the front of the pelvis (Figure 3):
- where the sartorius muscle joins to the ASIS (anterior superior iliac spine).
- where the rectus femoris muscle joins to the AIIS (anterior inferior iliac spine).
You can visit the “Soft Tissue Related Pain” tab to view these muscles.
The pain of apophysitis is related to an inflammation of the bony growth centres where these muscles attach. Pain is generally experienced locally at the area of muscle attachment but can radiate around the area as well.

Other growth-related bony issues:
- Perthes disease or Legg-Calvé-Perthes Disease – is misshaping of the femoral head related to issues with blood flow to the bone. Most common during ages 4-10 years.
- Slipped Capital Femoral Epiphysis or Slipped Upper Femoral Epiphysis-usually a small shift in the growth plate in the neck of the femur that can change the shape of the head and neck of the femur. Most common during ages 8-15 years.
Pain related to the bones could also be felt anywhere around the hip or pelvis region depending on the bone affected and the cause of the bone pain. Click on our Pain Locator Map to review the areas you feel pain and learn more about the bones that may be related to pain in each area.
- perform a thorough assessment and let you know if a bone issue may be suspected. In these cases, you may be advised to undertake further imaging or referral to a medical specialist for further advice
- provide or refer you for rehabilitation at an appropriate time following bony injury
- provide important information about managing sporting activity and recovery in those with bony stress injuries or adolescents with bony ‘growing pains’
- address muscular or biomechanical issues that may be contributing to bone-related pain, for example, running style may have an impact.



 Joint Related
Joint Related  Soft Tissue Related
Soft Tissue Related  Bone Related
Bone Related  Back Related
Back Related  Peripheral Nerve
Peripheral Nerve  Other causes
Other causes