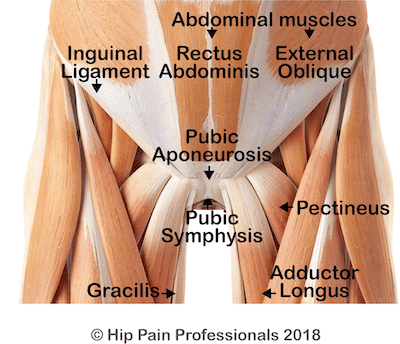
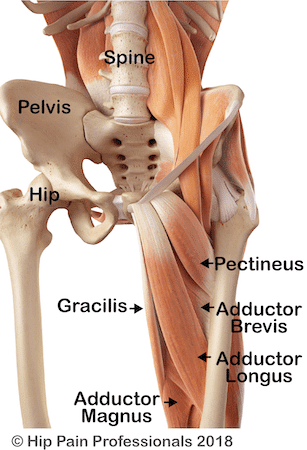
Adductor related groin pain is pain in the groin region (upper-inner thigh) related to the adductor muscles and their connections. Tears or strains may occur within the adductor muscles themselves; where the muscles and tendons join (musculotendinous junctions); or within the tendons (attaches the muscle to the bone).