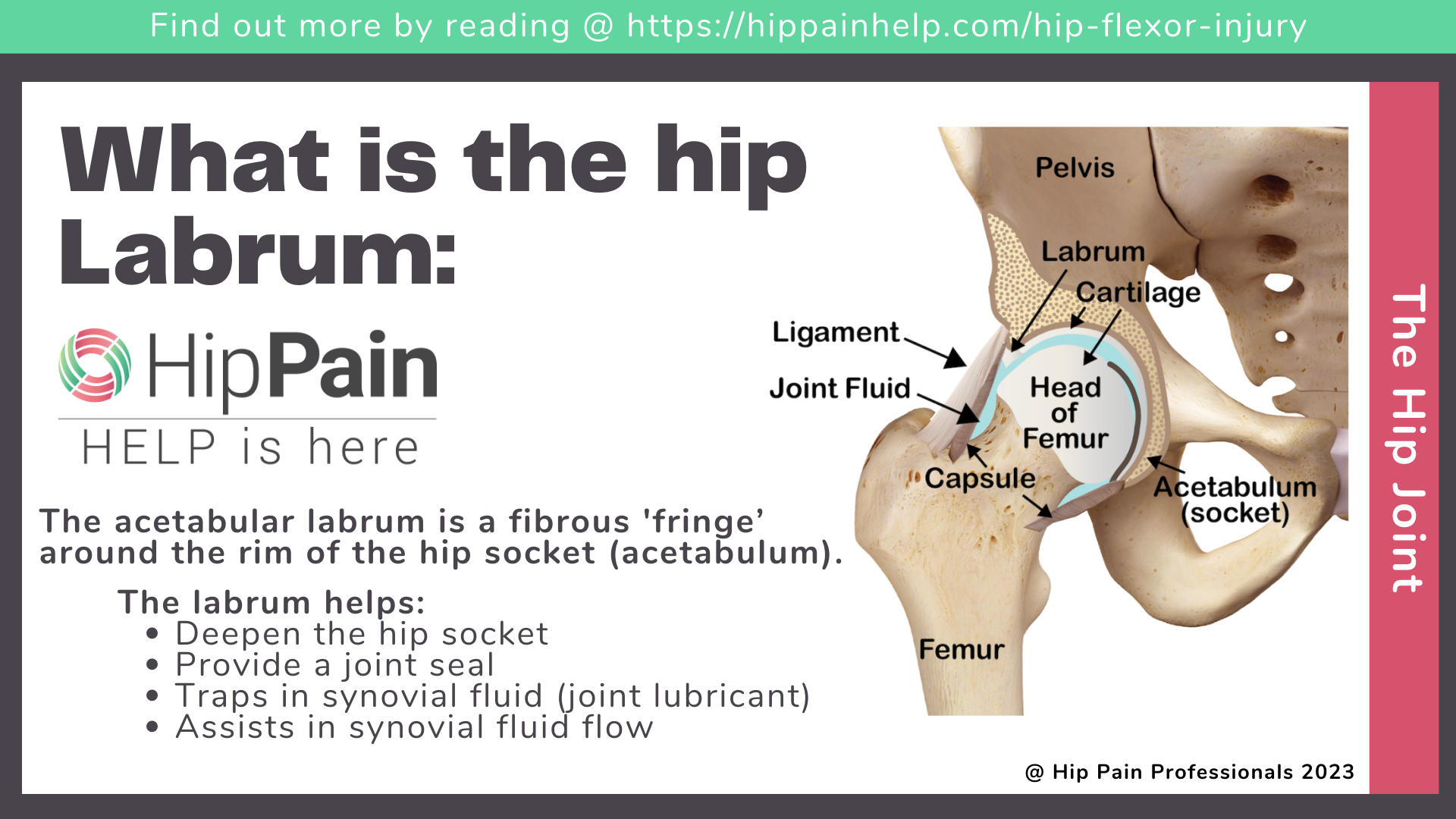
What is the labrum in the hip, and what does it do?
To understand what is a hip labral tear is let us first understand what the hip labrum is. The acetabular labrum is a fibrous ‘fringe’, a ring of cartilage that attaches around the rim of the hip socket (the acetabulum). It is most commonly triangular in shape, 2-3 mm thick and extends out from the acetabular socket 6-10mm. The labrum has a number of key functions.
The hip labrum:
- Deepens the hip socket joint
- Provides a seal for the joint, creating a vacuum that helps hold the ball (head of the femur) into the socket
- Traps synovial fluid (normal joint lubricant) between the ball and the socket This means that when walking and running, much of the landing forces are absorbed by fluid, rather than the joint cartilage
- Assists with flow of synovial fluid, important for cartilage nutrition within the hip joint
As the acetabular labrum is a structure at the edge of the hip joint, in most people the labrum only absorbs 1-2% of total joint load when standing.1 The main cartilage surfaces of the ball and socket take almost all of this load, and this is why it is common for people to have tears in their hip labrum without even knowing about it – more on that below.
How common is a labral tear of the hip and do they always hurt?
You might be surprised to learn that at least 50% of people without hip pain have a tear in the acetabular labrum, compared with around 62% of those with hip pain!2 So while it can cause pain, because the labrum does contain sense receptors,3 it doesn’t always become painful.
It often depends on what you are doing with your hips, and the natural bone shape of your ball and socket may play a role. If you’re regularly moving your hip into the very end of its range e.g., deep squats, lunges, splits or forced rotation, the labrum will absorb more load and a labral tear is more likely to become painful.
The labrum may also be exposed to higher loads in those with certain bone shapes – cam or pincer shape, or acetabular dysplasia (shallow socket). Read more about this in the next section.
This brings up 2 key points
- Just because a labral tear is detected on a hip scan, it doesn’t mean it is the source of pain. A good clinical assessment by a health professional experienced with hip pain is required. They can help determine whether the labral tear is likely to be relevant to your hip problem.
- Labral tears can be painfree. If you do have hip pain related to a labral tear, physical therapy (physiotherapy) can assist in helping you reduce time spent in irritating positions and improving how you control movement at the hip to alleviate pain related to the labrum.

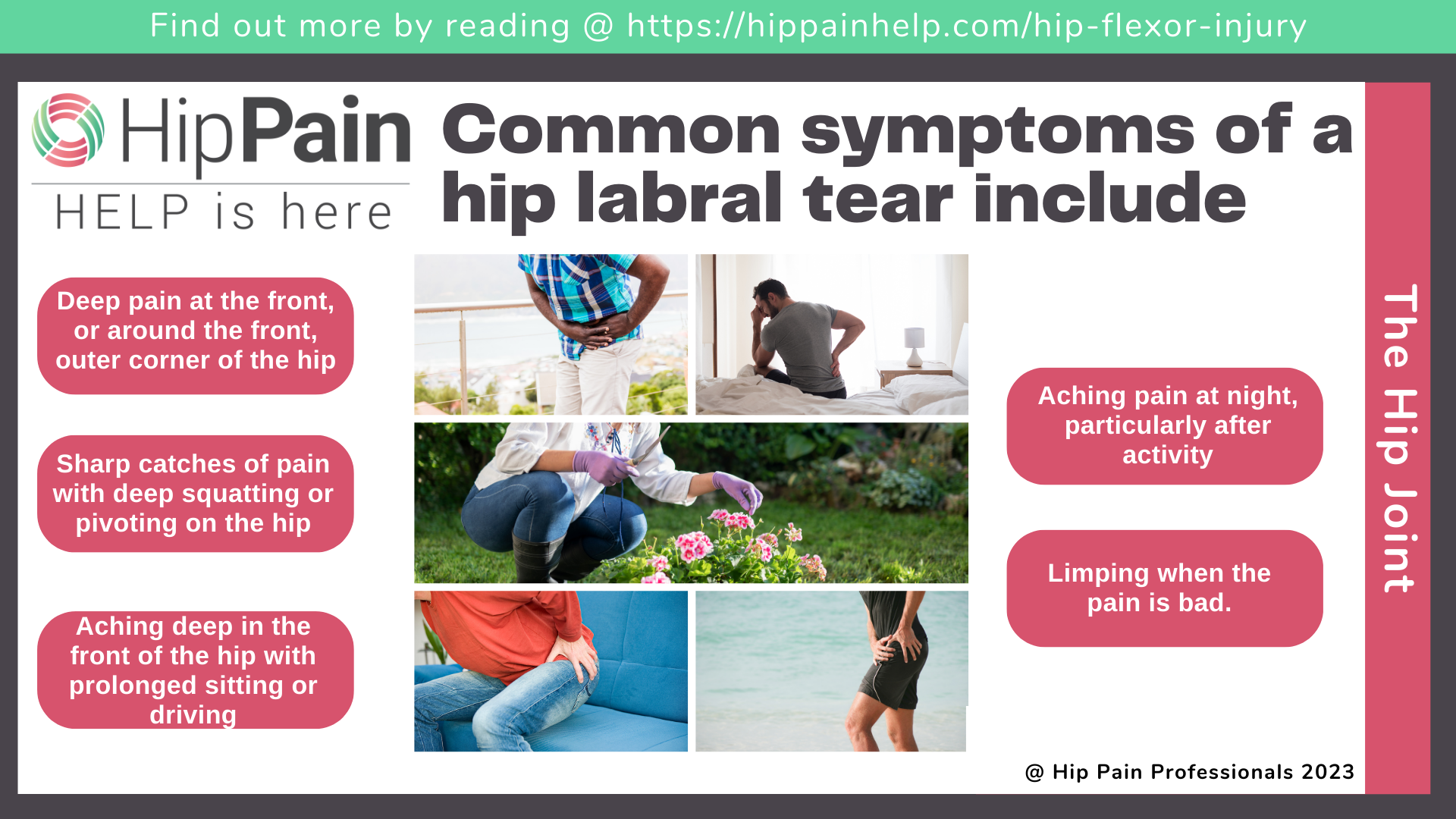
Symptoms of a hip labral tear
Common symptoms of a hip labral tear include:
- deep pain at the front (groin pain), or around the front, outer side of the hip,
- sharp catches of pain in a deep squat position or pivoting on the hip,
- aching deep in the front of the hip with prolonged sitting or driving,
- aching pain at night, particularly after activity,
- limping when the pain is bad
What causes a hip labral tear?
The labrum can sometimes be injured traumatically, most commonly with a sudden twist or pivot or during an extreme movement to the end of the joint range. However, medical researchers have discovered that acute trauma is the least likely cause of hip labral injury.
It is much more common that individual variations in bony and ligament structure increase the risk of micro-trauma to the labrum. Repeated small insults to the labrum over time may eventually result in a visible tear on Magnetic Resonance Imaging (MRI scan).
The development of an acetabular labral tear likely depends on your hip shape and what you are doing with your hips.
Bone shapes that may increase the risk of a hip labral tear
Acetabular dysplasia (a shallow hip socket)
Some people are born with a smaller or shallower hip socket that doesn’t provide as much bony coverage or support for the ball at the top of the femur (thigh bone). This is called acetabular dysplasia.
Less bone allows for greater flexibility and so it is not uncommon to find dancers, gymnasts and circus performers with this bone shape. However, less bone in the hip socket does mean that the acetabular labrum will need to do a little more work.
Remember we said that the labrum normally absorbs only 1-2% of total joint load? In those with acetabular dysplasia, the labrum absorbs 4-11% of total hip joint load,1 which is a dramatic increase.
The shallower socket also allows more gliding of the ball in the socket, which also needs to be controlled by the labrum. These extra loads may contribute to development of acetabular labral tears in people with acetabular dysplasia, and sometimes this may lead to pain. Again, what you do with your joint and how, will also influence the likelihood of developing pain.
Read more about the development, symptoms and treatment of acetabular dysplasia by clicking on the pink text.
Femoroacetabular Impingement (FAI)
Femoral acetabular Impingement (FAI) is a mismatch of the ball and socket of the hip joint, which may result in increased loads on the labrum of the hip.
Variation in the shape of the ball and/or the socket results in the bones coming together a little earlier than normal (femoroacetabular impingement) during hip flexion (knee to chest) or inward rotation of the hip. As the labrum is on the edge of the socket, it may be exposed to greater compression or shear force, particularly in extremes of joint motion.
Cam shape of the femoral head
Cam shape is where the ‘neck’ of the femur just below the head (ball) is thicker than average. This shape develops in adolescence and appears to be a natural response to higher levels of participation in weightbearing sports that involve change of direction.
The neck of the femur becomes thicker and stronger, but the extra bone means the thicker neck will impinge against the socket earlier in hip motion, increasing load on the labrum.
Pincer shape of the hip socket
Pincer shape is where the socket is deeper or facing slightly less forward than typical. This means there is relatively more bone at the front of the socket and so once again, the bones come together earlier with more potential load on the labrum.
However, while there are links with cam shape and increased risks of developing hip pain, the relationship between pain and pincer morphology is not strong.
Mixed FAI
A mix of cam and pincer shape that results in early bony impingement is called “mixed FAI”.
Other possible contributors to hip labral tears
The research has shown that although people with acetabular dysplasia and FAI may be at higher risk of developing hip pain associated with a tear of the hip labrum, only some people with these bone shapes ever develop a problem.
Why is that? Well, it’s because it is not just about bone shape and we probably don’t fully understand all the possible factors and their relative importance yet.
But what you do with your hip and how you control hip movement are thought to be 2 important factors.
People that repetitively force their hips into the very end of their range, particularly with added load or at higher speeds, may overload the labrum. Reduced muscle strength and co-ordination around the hip may also result in higher loads being transmitted across the joint and the labrum.
Pair one or both of these things with one of the bony variations we’ve mentioned, dysplasia or FAI, and the risks of pain related to a labral tear are likely to be substantially increased.

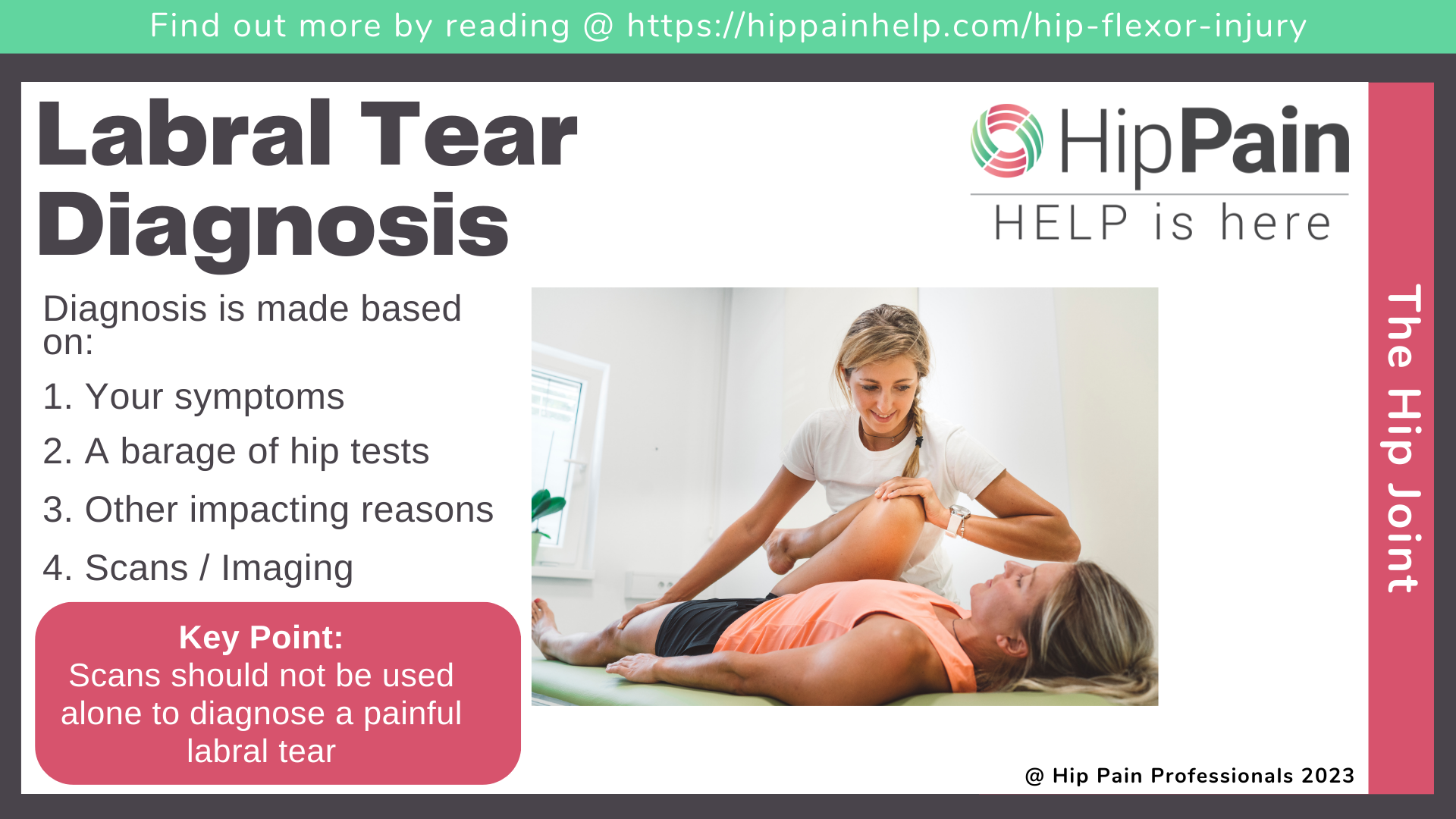
Diagnosis of a painful hip labral tear
To diagnose a labral tear, a health professional will first ask you about the location, type and behaviour of your pain, the history of your condition, what types of activities you do normally and which of these appears to aggravate your hip.
The health professional will also assess your hip range of motion (flexibility) and perform some special tests that provide some guidance as to whether you are likely to have a labral tear.
Often the final diagnosis is made on imaging (scans), however, remember these are not a great way to make a diagnosis by themselves (because lots of people have labral tears without hip pain. The clinical assessment by a health professional (interview and physical examination) can help to figure out if a labral tear seen on imaging is likely to be the source of your problem.
Scans should not be used alone to diagnose a painful labral tear
This is only one part of the assessment – the diagnosis is only the beginning. The health professional then needs to perform other assessments of the hip, your whole lower limb, the way you move and how your muscles are functioning.
They may also want to assess your sporting technique and/or ask some detail about your normal training routine and any recent changes to your training schedule.
All of this additional information helps to build a picture of the factors that are most likely to have contributed to the development of your hip pain.
What is the usual treatment for a hip labral tear?
What can you do about a labral tear? Lots of people with a labral tear can continue in life without issues, even competing in sport to a high level.
If pain does develop, the first thing to try is a program of rehabilitation, usually with a physical therapist (physiotherapist). Just having a tear, does not mean you need to jump straight to a surgical treatment, as a labral tear can settle and become painfree again with rehabilitation. For those who continue to have problems, there are additional medical options.
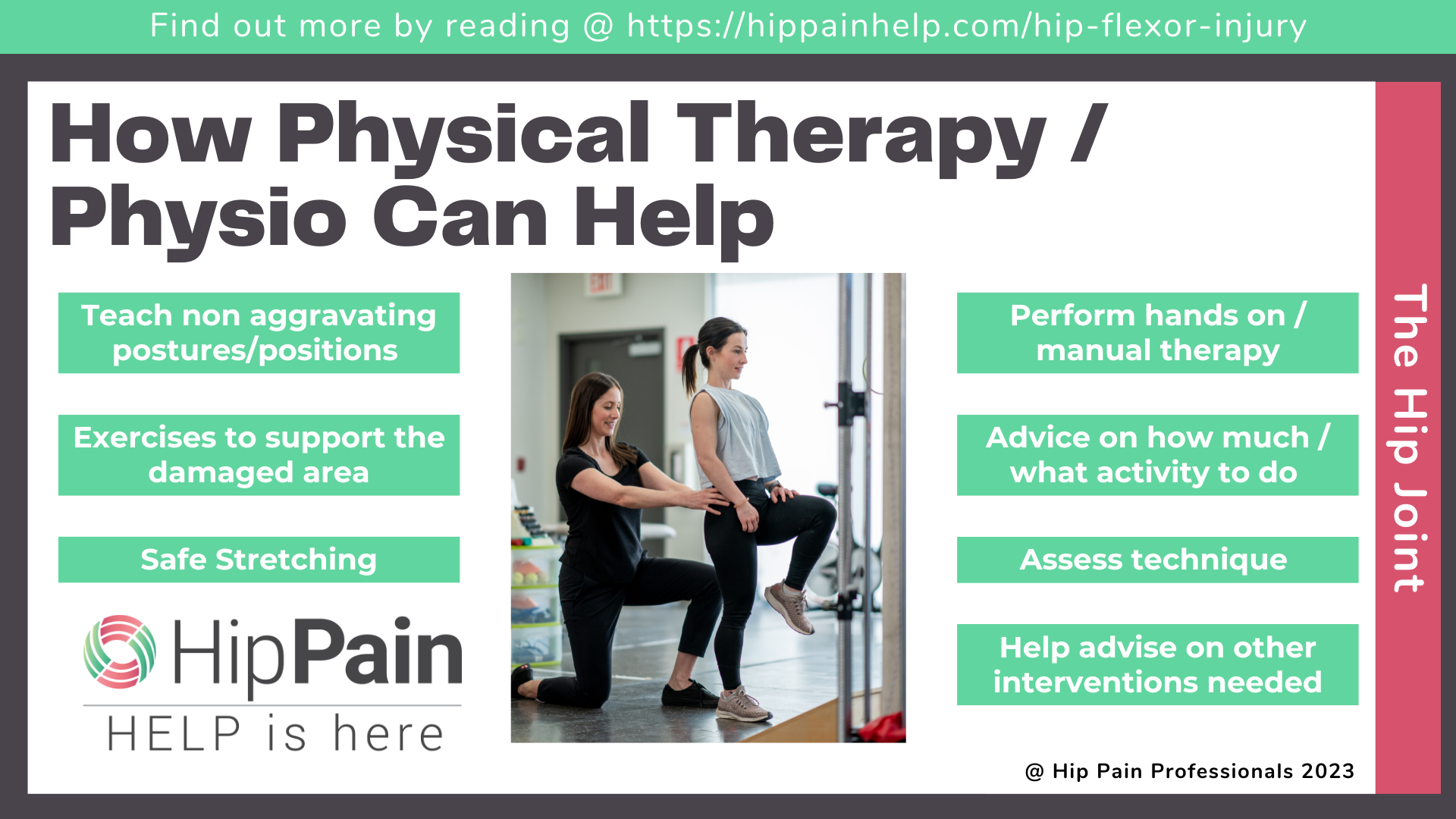
Physical therapy treatment for a hip labral tear
The 2 main components of a rehabilitation program for a painful labral tear are education around hip care, and an individualized exercise program.
Learning to care for your hip
Learning to care for your hip and how to reduce unnecessary load on your labrum is one of the most important components of any rehabilitation plan. You can do all the exercises you like, but if you don’t understand why your labrum is becoming painful and how to control this, you are likely to continue experiencing flares of pain.
The advice will be a little different, depending on what the health professional has discovered in your examination about your likely bone shape, work environment, car, sport or recreation, training habits etc, etc. Getting individualized advice will be most helpful.
Often the best places to start is in modifying things that you might be doing a lot – sitting, walking, running. Simple modifications to these high-duration positions or high-volume activities can often make a big difference.
You can find some great advice in other blogs on this site about:
Exercise for a labral tear
Your physical therapist, physio or exercise physiologist may develop a specific exercise program with hip exercises to help reduce your pain and regain your normal function in your hip.
This rehabilitation program will also be most effective when tailored to the individual. For example, a program for someone with a labral tear and acetabular dysplasia will be a little different to that for someone with FAI. A program for an athlete will also be a little different to that for someone who has lower levels of physical activity.
Generally, the program will involve helping you to move in ways that avoid repetitive overload of the labrum, and teach you the best exercises to help address any specific weaknesses or reduced coordination you may have in the muscle around your hip. Ensuring good strength, endurance and control around the trunk, knee and ankle is also often important to help reduce excessive loads crossing the hip. You will be guided in flexibility exercises to help, as well as those to avoid that may irritate the hip labral tear symptoms further.
Deep muscles around the hip will be important to provide support to the joint, and the gluteals, hip flexors, thigh, calf and abdominal muscles will also be important in better sharing loads across the hip joint and across the whole lower half of the body.
Other physical therapy treatments
Hands-on treatments, or manual therapy, to relieve muscle tension may be provided and acupuncture or needling techniques are also sometimes used to help reduce pain. These treatments may be effective for some people in achieving some short-term relief while they work on the 2 main strategies – hip care and an exercise program.
A physical therapy rehabilitation program for a painful labral tear is more likely to be successful when developed by a physical therapist or physiotherapist who understands labral tears and can develop an individualized program to suit your situation.