Pain at the side of the hip related to trochanteric bursitis and/or gluteal tendinopathy is one of the most common musculoskeletal conditions experienced by post-menopausal women. It can also affect younger women and males, although less commonly. With substantial effects on sleep, activity levels, and quality of life, it's no wonder that doctors and patients alike, often opt for cortisone injections for trochanteric bursitis and gluteal tendinopathy.

Do you have hip bursitis or gluteal tendinopathy? Not sure where to start on your road to recovery? Or what your next steps should be?
This FREE resource provides a suggested treatment pathway, based on the available scientific evidence and Dr Alison Grimaldi's 30+ years of clinical practice as a physiotherapist and 20+ years as a researcher and educator in this field.
Recovering from Gluteal Tendinopathy, Trochanteric Bursitis or GTPS
FIRST LESSON IS FREE!
Reduced health in the gluteal tendons (fibrous structures that join the gluteal muscles to the top of the femoral bone) and trochanteric bursae (thin pockets of fluid that help the tendons slide between other structures) may become painful in some people. This is sometimes referred to as Greater Trochanteric Pain Syndrome – GTPS.
If you’d like to read more about the differences and causes of trochanteric bursitis, gluteal tendinopathy and GTPS, click on the coloured text in this sentence. If you then want to find out more about whether cortisone injections are a good treatment option, jump back to this blog.
In this blog, we’ll take a close look at cortisone injections for trochanteric bursitis and gluteal tendinopathy, covering the following main topics:
Corticosteroids are a family or ‘class’ of drugs that mimic naturally occurring hormones, called glucocorticoids. Glucocorticoids are primary stress hormones, like cortisol, that regulate a variety of bodily processes and are essential for life.1
Glucocorticoids control inflammation generated by the immune system in response to injury or illness. Inflammation is an important part of natural healing after injury but as they say, all things in moderation! Our hormones help to control the process.
Manufactured corticosteroids are thought of as powerful anti-inflammatories, working by suppressing the immune system. This might be helpful in systematic inflammatory health conditions such as rheumatoid arthritis, inflammatory bowel disease, lupus, skin conditions such as eczema or psoriasis, or lung conditions such as asthma or chronic obstructive pulmonary disease.
The most common corticosteroid drugs include:


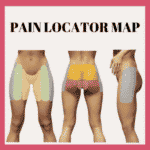
If you have pain directly over the prominent bone at the side of the hip, and you are tender here to touch or lie on your side, you may well have this condition.
We have prepared a self-test in the first FREE LESSON of our self-help course.
You can find it here:

Do you have hip bursitis or gluteal tendinopathy? Not sure where to start on your road to recovery? Or what your next steps should be?
This FREE resource provides a suggested treatment pathway, based on the available scientific evidence and Dr Alison Grimaldi's 30+ years of clinical practice as a physiotherapist and 20+ years as a researcher and educator in this field.
Injected corticosteroids, usually just referred to as ‘cortisone injections’ are used frequently for painful tendon and bursal conditions. So, how do cortisone injections for trochanteric bursitis and gluteal tendinopathy work? By reducing inflammation, you might say!
Well, despite the persistent term trochanteric burs-‘itis’ and the older term, gluteal tendin-‘itis’ (‘itis’ meaning inflammation), these conditions are rarely truly inflammatory.
Microscopic examination of the bursa in trochanteric bursae surgically removed because of ‘bursitis,’ did not find any inflammatory cells or indications of a true inflammatory process.2 The term ‘tendinopathy’ is now preferred over ‘tendinitis’ due to the current understanding that the condition is rarely related to an inflammatory process.3
So, how can cortisone help if it’s not about inflammation?
For over 20 years, many researchers and health professionals have been raising questions about why corticosteroids are being used for tendinopathy, if and how they help, and if it’s such a good idea.4
Where the pain comes from in tendinopathy is a complex question, but changes in the production of certain chemical messengers (cytokines), may stimulate pain receptors in the tissues.5 Corticosteroids act to reduce the production of these cytokines, which is possibly an important mechanism for how they reduce pain in tendinopathy and bursitis.
But for how long does it help, and is it really helpful or harmful to the health of your tissues? Let’s take a look.


Recovering from Gluteal Tendinopathy, Trochanteric Bursitis or GTPS
FIRST LESSON IS FREE!

Do you have hip bursitis or gluteal tendinopathy? Not sure where to start on your road to recovery? Or what your next steps should be?
This FREE resource provides a suggested treatment pathway, based on the available scientific evidence and Dr Alison Grimaldi's 30+ years of clinical practice as a physiotherapist and 20+ years as a researcher and educator in this field.
Most studies show that cortisone injections for trochanteric bursitis and gluteal tendinopathy result in at least partial pain relief, for at least a short time, in most people.
Our study, the LEAP trial, showed that an evidence-based education and exercise program for gluteal tendinopathy (+/- trochanteric bursitis) was more effective than a corticosteroid injection at reducing pain at 8 weeks.6
Trial participants who were given education and exercise were also around 20% more likely to rate their outcome as successful in both the short (8 weeks) and long term (1 year) than those who had a cortisone injection.6
Another study showed that cortisone injection provided no greater relief than a placebo saline (salty water) injection in either the short-term (4 weeks) or longer-term (6 months).7 So, is it worth the risk?


While they may reduce pain to some degree in the short term, it is important to be aware that injected corticosteroids are toxic for tendon cells, and the bursa and skin and bone …
Cortisone reduces the production of new tendon cells and collagen fibres, potentially resulting in weaker, less healthy gluteal tendons.8 Even when the cortisone is injected into the bursa, it will still affect the neighbouring gluteal tendons.
A cortisone injection for trochanteric bursitis and gluteal tendinopathy is often given to provide a 'pain-free window of opportunity' in which to rehabilitate. But in fact, cortisone injections may hinder rather than help your rehabilitation.
For tendinopathy at the elbow, adding cortisone to a rehabilitation program reduced and delayed the effects of an exercise program.9 Cortisone may reduce the benefits of an exercise program for a mix of reasons, including reduced tissue health and differences in behaviour.
If the pain of bursitis or tendinopathy is reduced almost immediately by cortisone injection and the usually accompanying local anaesthetic (also toxic for tendons), the person is much less likely to be mindful of looking after their tendon or bursa.
Let’s be honest, if the pain is reduced to a level that it can be fairly easily ignored, you’re likely to go back to doing all the things you need to do and want to do, without thinking too much about your hip. And if the pain’s not too bad and you are weighing up whether to do your rehab exercises or spend the time doing something else, rehab may get pushed down the priority list.
This is certainly what we see in our physiotherapy clinics - people who have cortisone injections are less likely to remember or prioritise the changes we’ve recommended and the exercise programs we’ve prescribed.
In our LEAP scientific trial of treatments for gluteal tendinopathy (+/- trochanteric bursitis), we found that those who had a cortisone injection were much less likely to abide by the advice provided. All groups (1. Education and Exercise; 2. Cortisone Injection; 3. Basic Advice Only) were advised to initially reduce activity levels and then gradually increase activity, allowing time for the tendons to adapt.6
The education and exercise group and the basic advice group did just that – we tracked their activity levels. However, those who had the cortisone injection generally ignored this advice and actually increased their activity levels immediately. Then at 4 weeks, when the effects of the cortisone started to wear off and for many pain returned, there was a pattern of activity levels dropping again and remaining lower over time. There were no statistically significant differences in activity between groups over time, but the overall patterns are consistent with what we see in clinic.
We see this again and again in the clinic - after a cortisone injection:
So, when the cortisone starts to wear off, usually in a few weeks, they are in a worse situation than before – the tissues are less healthy, and they have not addressed the underlying problem. However, because they received some welcome relief from the injection, many people will then head back to the doctor for another injection.


This can start a vicious downward spiral of repeat injections and reducing the health of the tissues, making it harder to achieve optimal results with rehabilitation. This may result in trying other treatments with less evidence and eventually more invasive treatments such as surgery.

Do you have hip bursitis or gluteal tendinopathy? Not sure where to start on your road to recovery? Or what your next steps should be?
This FREE resource provides a suggested treatment pathway, based on the available scientific evidence and Dr Alison Grimaldi's 30+ years of clinical practice as a physiotherapist and 20+ years as a researcher and educator in this field.
The truth is – WE DON’T KNOW!
When studies have looked at the 'safety' of cortisone injections they look at things like infection, allergic reaction, and tendon rupture (which has been reported for the Achilles tendon after cortisone injection). Tendon rupture after a single injection is rare but is more likely with multiple injections, where tendon health gradually reduces over time.
The general answer from our medical colleagues about how many cortisone injections are safe is ‘2-3 a year’, but this is a ‘rule of thumb’ and does not appear to be based on any scientific studies.
The safety threshold is likely to be different for different people and different levels of tendon health and general health, but we have no adequate guidelines to give you clear evidence-based advice about how much is safe.
What we can tell you from our experience, is that less is better, and none is better still!


If you’ve already had one or more cortisone injections for trochanteric bursitis and gluteal tendinopathy, just put that aside now as a treatment option, and focus on high-quality rehabilitation – work hard at it for 3-6 months at least, and then keep up a maintenance program at least twice weekly to keep those tendons as healthy as possible.
If you haven’t had any injections yet, do your best to avoid them. High-quality rehab, like the program we provided in the LEAP trial, can start turning things around for most people.
Evidence-based programs involve:
1. Education
You need to understand as much as you can about the condition and how to alter things in your everyday life that might be aggravating your tendon or bursal pain. Things that might contribute to this irritation include:
Understanding how to control loads on your tendons and bursae by managing your activity levels is also important – avoiding sharps peak in activity, and types of activities that are more likely to be aggravating.
2. Exercise
An evidence-based exercise program for gluteal tendinopathy and trochanteric bursitis has several aims:
You can find a high-quality program here on our site as a self-help program for recovering from gluteal tendinopathy, and trochanteric bursitis (GTPS). Or, visit our Hip Pain Professional Directory to see if you can find a physiotherapist or physical therapist with knowledge of this program near you, to help you through your rehabilitation.
Other treatments include shockwave therapy and platelet-rich plasma (PRP) injections, which have some (but not strong) evidence for medium to longer-term benefit, with surgery usually offered as a last resort if other treatments have not helped.
We wish you all the best in your journey and hope this has provided some insights about decisions around cortisone injections for trochanteric bursitis and gluteal tendinopathy. We hope you will agree that it’s a good idea to avoid these or keep them to a minimum and focus on high-quality rehabilitation for your gluteal tendinopathy or trochanteric bursitis.
Recovering from Gluteal Tendinopathy, Trochanteric Bursitis or GTPS
FIRST LESSON IS FREE!

Do you have hip bursitis or gluteal tendinopathy? Not sure where to start on your road to recovery? Or what your next steps should be?
This FREE resource provides a suggested treatment pathway, based on the available scientific evidence and Dr Alison Grimaldi's 30+ years of clinical practice as a physiotherapist and 20+ years as a researcher and educator in this field.
If you'd like a physiotherapist/physical therapist/rehab professional that knows hips to guide you through a recovery program, you can find the location of our Hip Pain Professionals below.
Top Tips for Hip Pain Relief Sitting, when Socialising or Travelling
Top Tips on Hip Pain Relief Sleeping
3 Simple Strategies to Reduce Hip Pain with Walking and Running
This blog was written by Dr Alison Grimaldi, physiotherapists, researcher, and educator, who has over 30 years professional clinical experience, dealing with patients suffering from a wide range of hip and pelvic conditions.

Dr. Alison Grimaldi BPhty, MPhty(Sports), PhD, FACP is a fellow of the Australian College of Physiotherapists, Practice Principal of PhysioTec Physiotherapy, an Australian Sports Physiotherapist , an Adjunct Senior Research Fellow at the University of Queensland, as well as an author and global educator
References