What is Hip Osteoarthritis?
Hip osteoarthritis (hip OA) is a condition that makes the joint painful and stiff. Osteoarthritis is the most common form of arthritis. There are other forms of arthritis that may be related to a systemic health condition, such as Rheumatoid Arthritis. Treatment will be different, so it is always important you know what type of arthritis you have. Discuss this with a health professional. Here, we will only discuss osteoarthritis.

Hip osteoarthritis is associated with reduced health of the joint structures. The hip joint is a ball and socket joint (Figure 1). The bones on both sides of the joint are lined with smooth cartilage (Figure 2). Hip OA is usually a slowly progressive condition, where the thickness and smoothness of the cartilage gradually reduces. In more advanced situations, the body lays down some extra bone, in an attempt to repair the area. This can be one of the reasons movement becomes restricted.
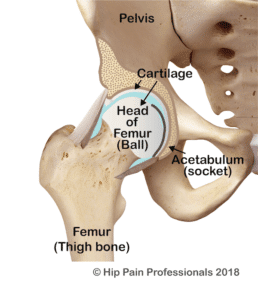
Figure 2: The hip joint, viewed from the front, cross section through the joint.

How is Hip OA Diagnosed?
diagnosis is usually reached through patient interview regarding symptoms and a physical examination conducted by a qualified health professional. An X-ray may be requested if the health professional feels it is important to determine the stage of the joint changes.
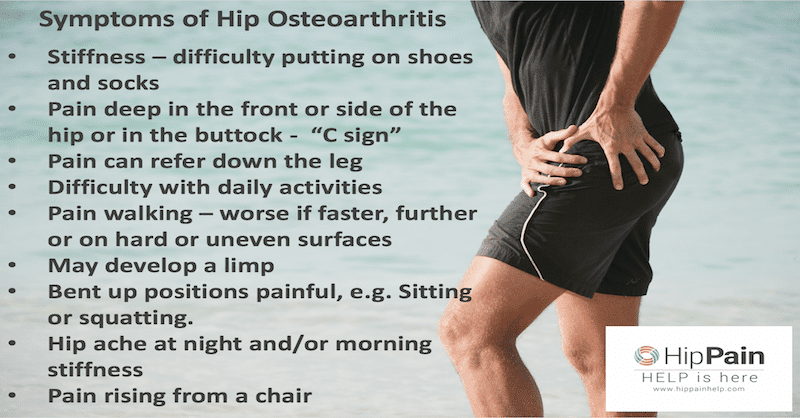
What are the usual symptoms of hip OA?

- One of the most common symptoms is stiffness: typically, people report they are having difficulty putting their shoes and socks on or cutting their toe-nails.
- Pain is generally felt deep at the front and/or buttock or side of the hip. A person with hip OA may describe the area of pain by grasping the side of their hip with their hand in a ‘C’ shape (referred to as the ‘C’ sign), or indicate a point deep between the front, back and side of the hip (the triangulation sign).

- Pain may also extend down the thigh, most commonly down the front of the thigh to the knee and also into the front/outer side of the shin. In some cases, people only feel the pain in the thigh, knee or shin, without hip pain.
- The ability to engage in activity or perform everyday tasks can become difficult, either due to the stiffness or pain.
- Walking may become painful, particularly longer distances, at a faster pace, on uneven surfaces, or on hard floors such as in shopping centres.

- A limp may develop in walking, with pain as weight is transferred onto the sore side and particularly as the leg moves backwards to push off. This may result in a lurching pattern where the body moves over to the side, to reduce load on the painful side.
- Positions where the hip is bent up can also aggravate the pain, such as prolonged sitting especially on a low chair or in a car or squatting to reach the ground, such as in cleaning or gardening.
- The hip may ache at night and stiffness is often worst first thing in the morning or when rising from a chair to walk.

What causes hip OA?
- Hip OA is a common condition worldwide. There is usually not a single cause but a combination of factors that increase the risk of developing OA. Age is a well-established risk factor for hip OA, with likelihood of developing signs of OA increasing with advancing age. However, it is possible for younger people to also develop OA if they have other strong risk factors.
- Genetics may also play a role – likelihood of developing OA is increased if other family members have had OA.
- Developmental disorders such as congenital hip dislocation, acetabular dysplasia, slipped capital femoral epiphysis and Perthes disease have all been shown to be associated with higher hip OA rates.¹
- More recently, femoroacetabular impingement (FAI) has been implicated in increasing the risk of hip OA.¹
- Obesity places higher loads on weightbearing joints such as the hips and knees. Carrying excess weight is thought to increase the rate at which the arthritis progresses.
- Previous hip joint injury or surgery can both increase the likelihood of developing hip OA.²
Your Hip Pain Professional Can:
- assess your unique case and discuss with you in hip osteoarthritis may be involved with your hip pain
- help guide you as to whether further imaging or blood tests may be required to confirm or further investigate your situation
- educate you about your symptoms, the causes and possible ways to manage your pain
- discuss treatment options for hip osteoarthritis with you (you can read more about this in our next blog)
- work with other hip pain professionals so help ensure the best management of your situation. This may be including hands on treatment, exercise, diet, education and maybe other further interventions
References
- Harris-Hayes, M. and Royer, N. (2011). Relationship of Acetabular Dysplasia and Femoroacetabular Impingement to Hip Osteoarthritis: A Focused Review. PM&R, 3(11), pp.1055-1067.e1.
- Richmond, S., Fukuchi, R., Ezzat, A., Schneider, K., Schneider, G. and Emery, C. (2013). Are Joint Injury, Sport Activity, Physical Activity, Obesity, or Occupational Activities Predictors for Osteoarthritis? A Systematic Review. Journal of Orthopaedic & Sports Physical Therapy, 43(8), pp.515-B19.