Gluteal Tendinopathy, Trochanteric Bursitis, Greater Trochanteric Pain Syndrome
– Are they all the same thing?
Pain over the outer side of the hip is commonly related to the way that the muscles, tendons and bones in this area interact. There is a part of the thigh bone (femur) that is more prominent at the side of the hip. This is called the greater trochanter. Most of the muscles that help you balance when you are standing on one leg either join onto or pass over this bony area. The deep gluteal muscles join onto the bone via fibrous tendons. Small flat ‘cushions’ called bursae reduce friction between the bone, the tendons and the overlying fibrous Iliotibial band that runs from the pelvis to the knee (a lot of anatomy to take in? – this is important to remember for the next part so hang in there…).
As all of these structures are so closely packed together, one or more of them may be irritated by the same activities or positions. Pain in the area may be described with different names depending on where you live and who has diagnosed you. The condition may be diagnosed as:
- gluteal tendinopathy
- gluteus medius or minimus tendinitis
- trochanteric bursitis or just hip bursitis
- Greater Trochanteric Pain Syndrome (GTPS) (which just refers to any irritated tissues over this bone).
Regardless of which term your health professional has used, the underlying causes for the pain are usually the same, so let’s move on to discussing this in more detail.
Gluteal Tendinopathy, Trochanteric Bursitis, Greater Trochanteric Pain Syndrome – What Are The Causes?
Many factors influence the health of the tendons and bursae, but either too much or too little stimulus may cause reduced health over time. Particular forces or loads may be more problematic than others.
The way you sit, stand, walk or run may contribute to gluteal tendinopathy and hip bursitis
Compression of the gluteal tendons may occur as the tendons wrap around the outer surface of the greater trochanter – the part of the femur (thigh bone) into which they are anchored. An increase in tension (stretch) in the overlying Iliotibial band may further increase compression of the tendons and bursae that sit between the band and the bone.
Positions where the knee crosses the body, or the hip is shifted out to the side will increase the tension in the iliotibial band and therefore the compression of the tendons and bursae at the greater trochanter.
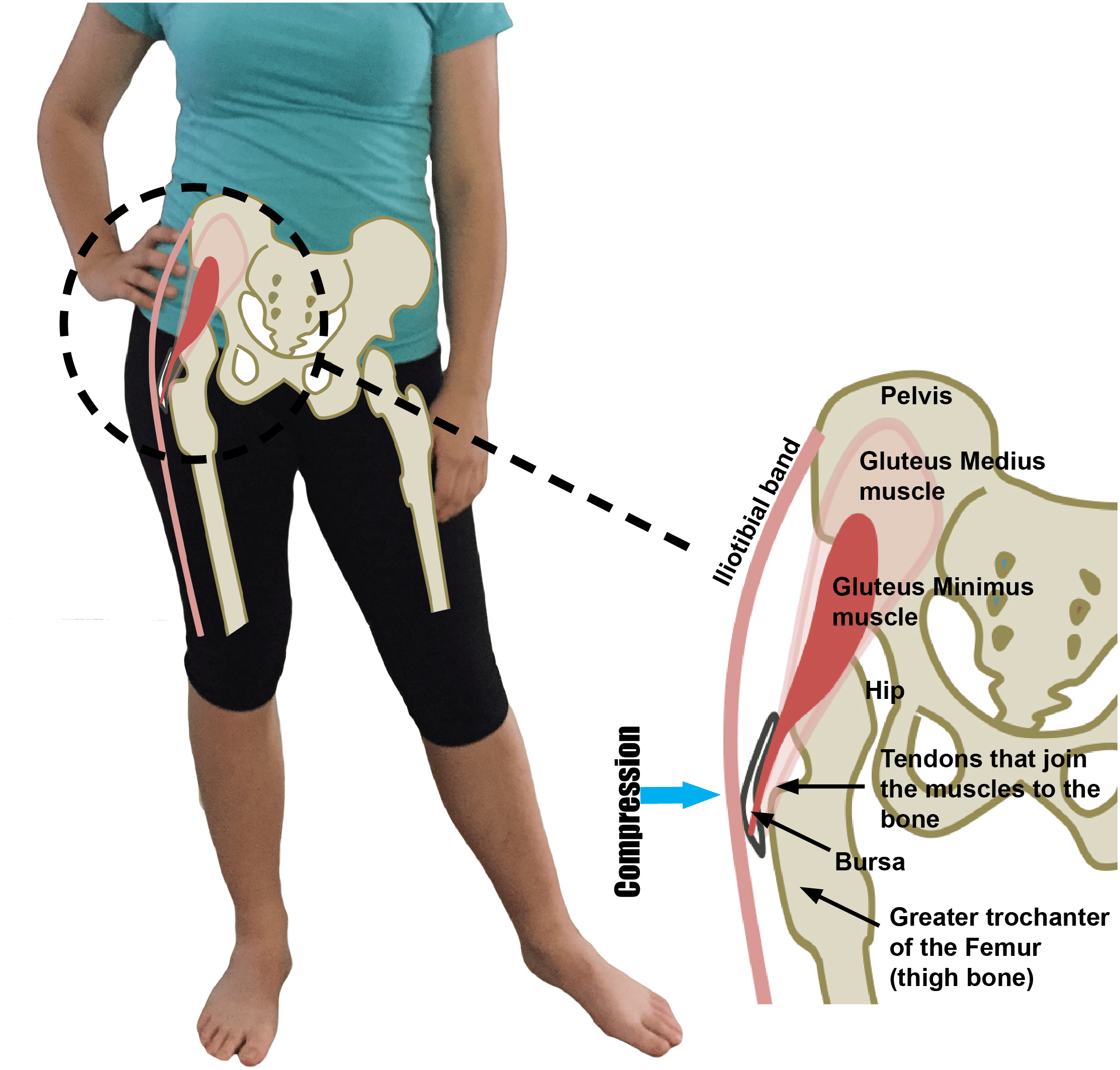
Compression of the gluteal tendons occurs as the tendons wrap around the outer surface of the greater trochanter into which they are anchored. Positions where the knee crosses the body or the hip is shifted out to the side, increase the tension in the band, compressing the tendons and bursae that sit between the band and the bone.1
- Postural habits such as hanging on one hip (as pictured here) or sitting with the knees crossed, place some tension and higher compressive loads on the tendons.
- Poor control of pelvic position (hip sagging and shifting) when walking, climbing stairs, running and squatting may also lead to excessive levels of compression and tension, potentially reducing health of the tissues.
All of these factors can be involved with your gluteal tendinopathy or trochanteric bursitis.
Changes in the health of the gluteal tendon and trochanteric bursa usually develop over many years. The tissues become less able to tolerate physical loads and pain may develop. Pain is the body’s way of warning us that we may not be coping with current loads.