Which Hip Replacement Surgery is best? Which hip prosthesis, meaning hip implant or artificial hip, is best? These are the two questions many people ask when the time comes to consider a total hip arthroplasty – the surgical term meaning total hip replacement surgery. This blog will explore the best materials and procedures for hip replacement surgery.
Most people will be wondering which hip surgery has the best success rate, which are the most successful procedures, and which is the best material to use for a new hip. But the answers can be very different depending on each individual. There is no one glove (or prosthesis) that fits all. We’ll be diving into the detail of everything you need to consider right here.
This blog will cover the following key considerations:
- The different surgical procedures, and when and why they may possibly be the best option.
- The options of conventional total hip replacement surgery versus hip resurfacing. the different approaches used when actually doing the hip replacement surgery, from the back or “posterior approach” versus from the front, the “anterior approach.”
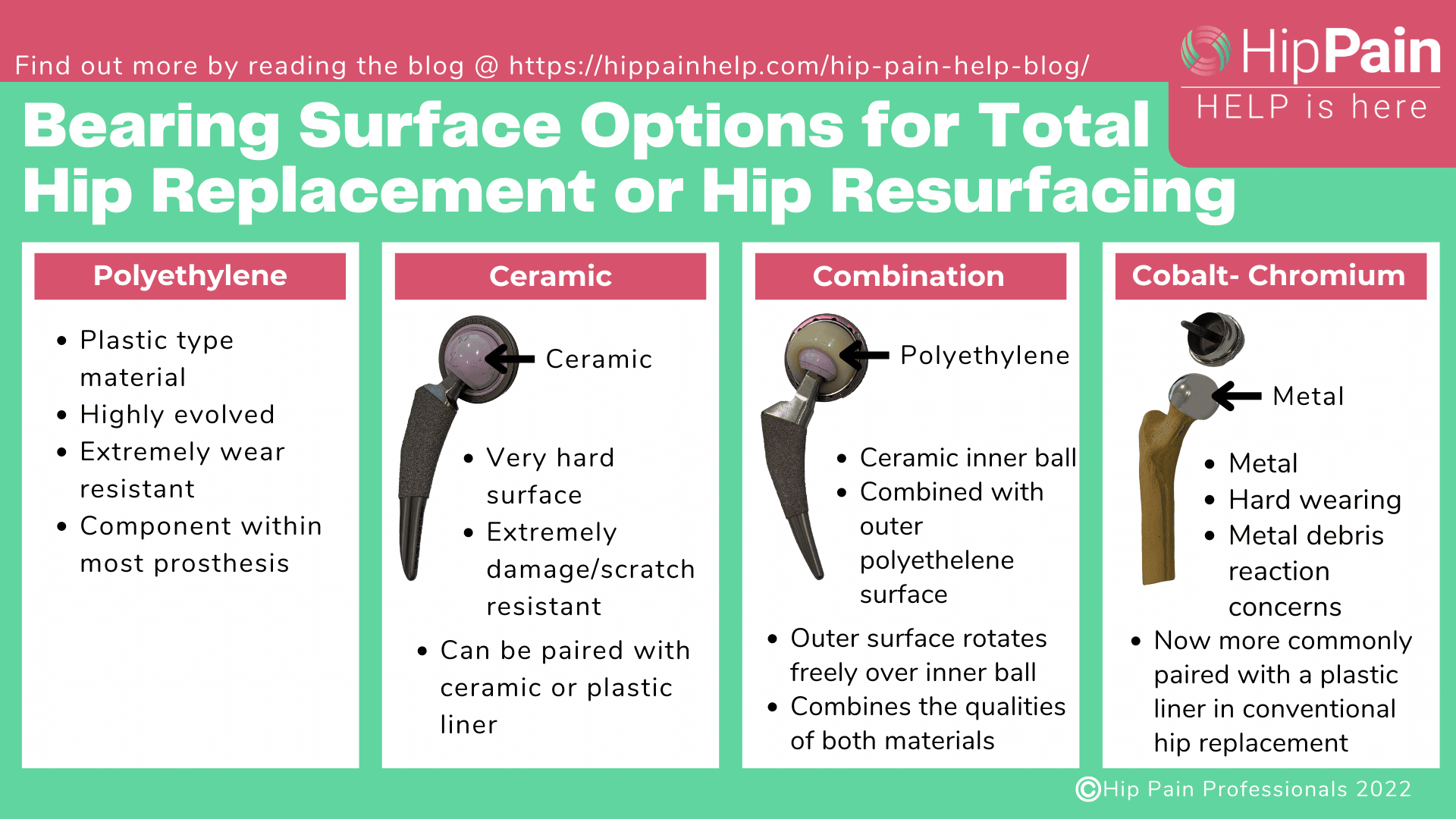
- The different hip replacement implants and the pros and cons of new implant options – which might be the best material and why.
It should be noted that all other non-surgical options to manage your hip pain, from physical therapy and exercise, weight management, through to other medical options, such as medication and hip joint injections (for example corticosteroid injections) should be exhausted before hip replacement surgery is considered.
Surgical Options for Total Hip Replacement
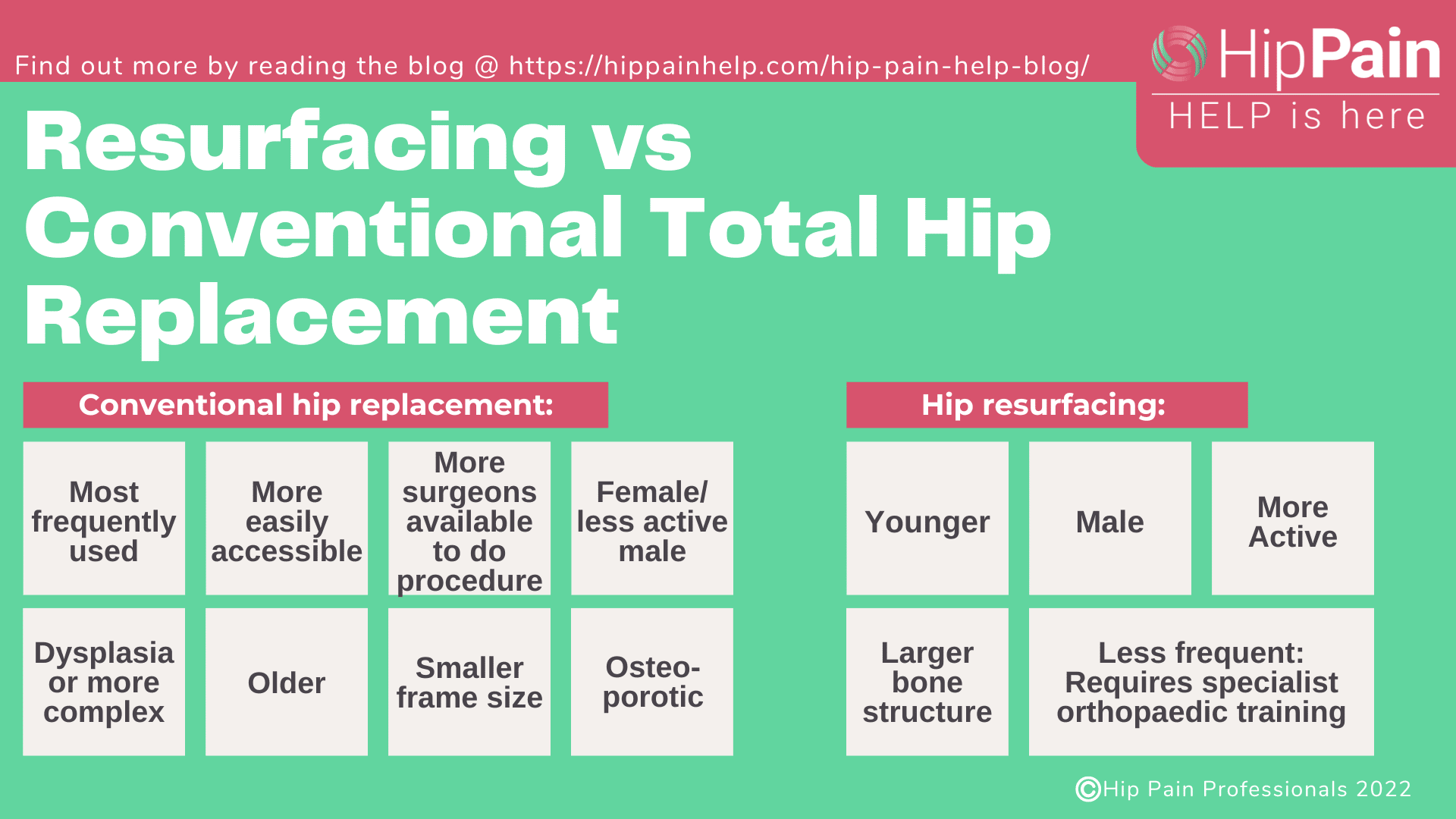
There are two main surgical options when hip replacement surgery is being considered. You can discuss both with your orthopaedic surgeon so that you can better understand which option is best for you and why. The options are Conventional Total Hip Replacement Surgery and Hip Resurfacing.
Conventional Total Hip Replacement Surgery
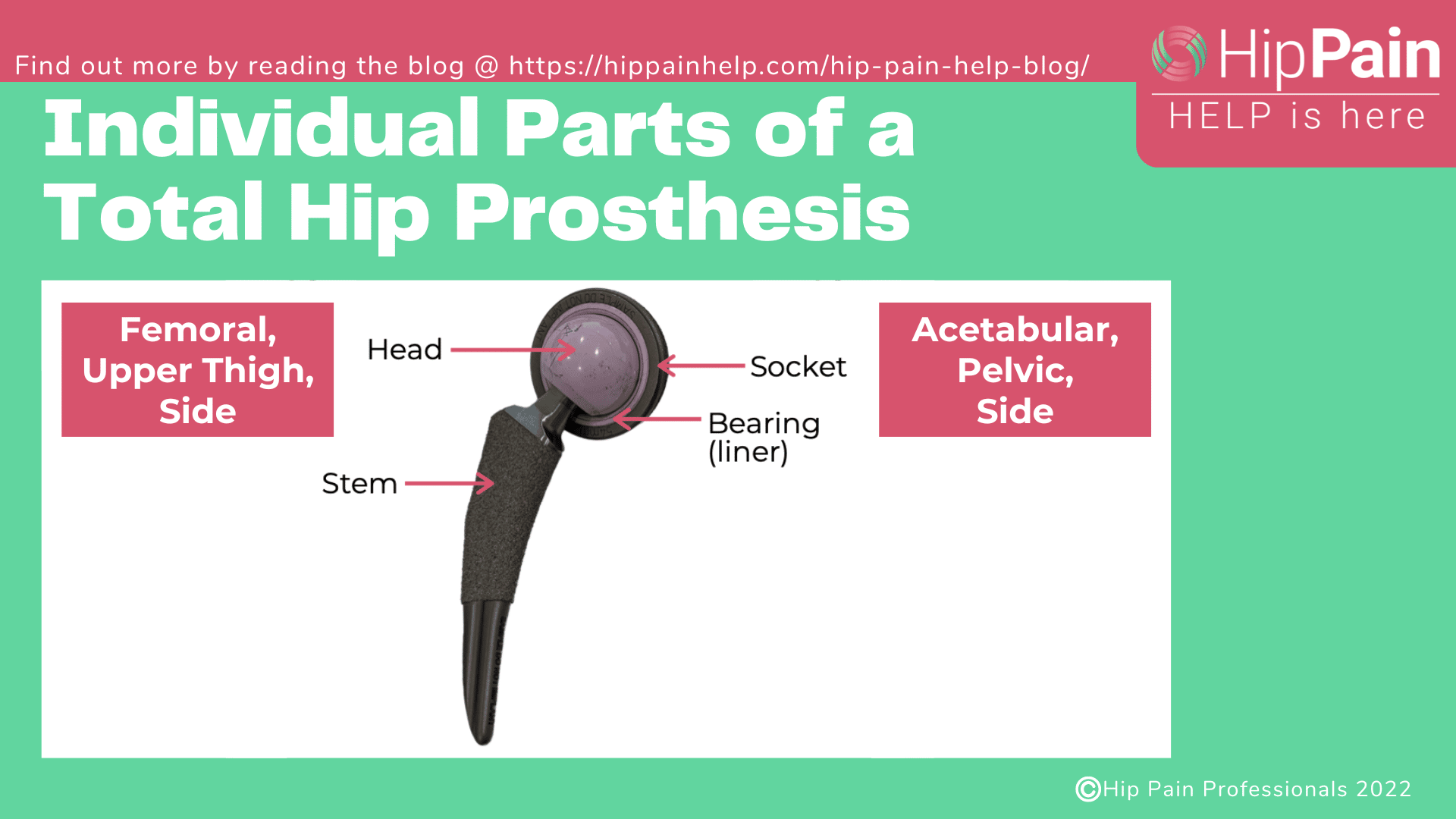
This is the most common procedure that will be used during Hip Replacement Surgery.1 It is the traditional hip replacement surgery. This makes up 98-99% of all hip arthroplasty surgeries for hip osteoarthritis. In a traditional total hip replacement, the head of the thighbone (femoral head) and the damaged socket (acetabulum) are both removed and replaced with metal, plastic, or ceramic components.
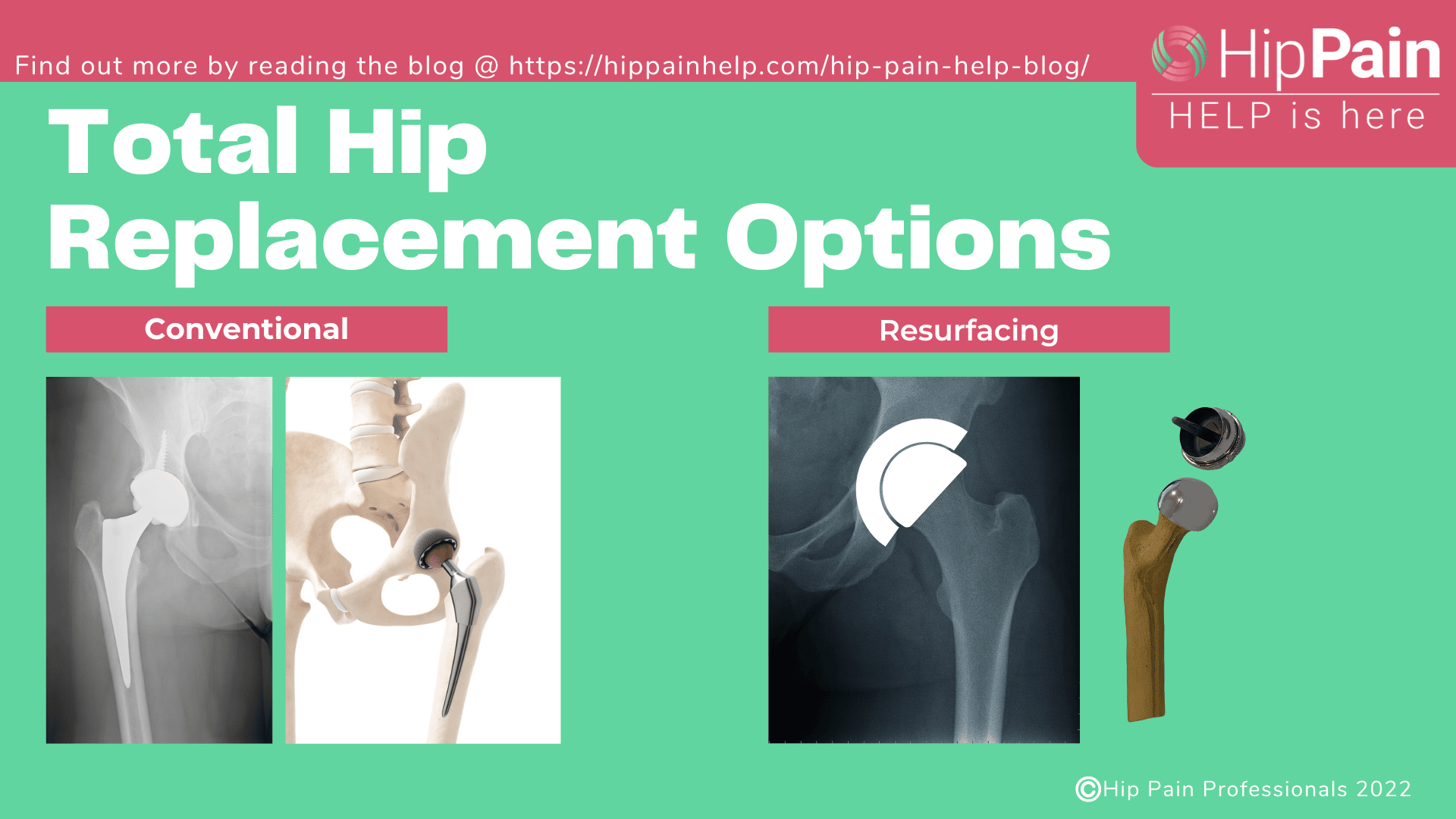
Hip Resurfacing
In a hip resurfacing procedure, the head of the thighbone (femoral head) is not removed. Instead, it is trimmed and then capped with a smooth metal covering, and the cartilage of the socket replaced with a metal lining Hip resurfacing implants have been in use in various forms for over 40 years, so it is not a new surgery.1 However, it is only an option for appropriately selected patients. Patients have to meet certain criteria to be eligible for the hip resurfacing implants.
Which total hip replacement surgery should you choose?
Two of the biggest factors in deciding on hip resurfacing or conventional hip replacement are age and activity levels. Hip resurfacing is often used in a younger, more active person as it is easier to do revision surgery in later years once the hip implant wears out.
Hip revision surgery means replacing the hip prothesis that is currently in place. Outcomes of revision surgeries are generally not as good as the first surgery, so the less procedures over your life, the better.
A Conventional Hip Replacement, although still the best option for most, is harder to revise when the hip replacement fails.
Assuming a long life, all hip replacements will eventually fail, most commonly due to loosening and wear, infection, fracture or dislocation.2 So, the age of the patient and when or whether they are likely to need a revision procedure is an important consideration when deciding what surgery, and when the surgery should be done.
How long does a hip replacement last?
The information available from joint registries have shown:
- 85% of prostheses last 20-years
- 58% of prostheses last 25-years
- Some have even lasted 40 years!2
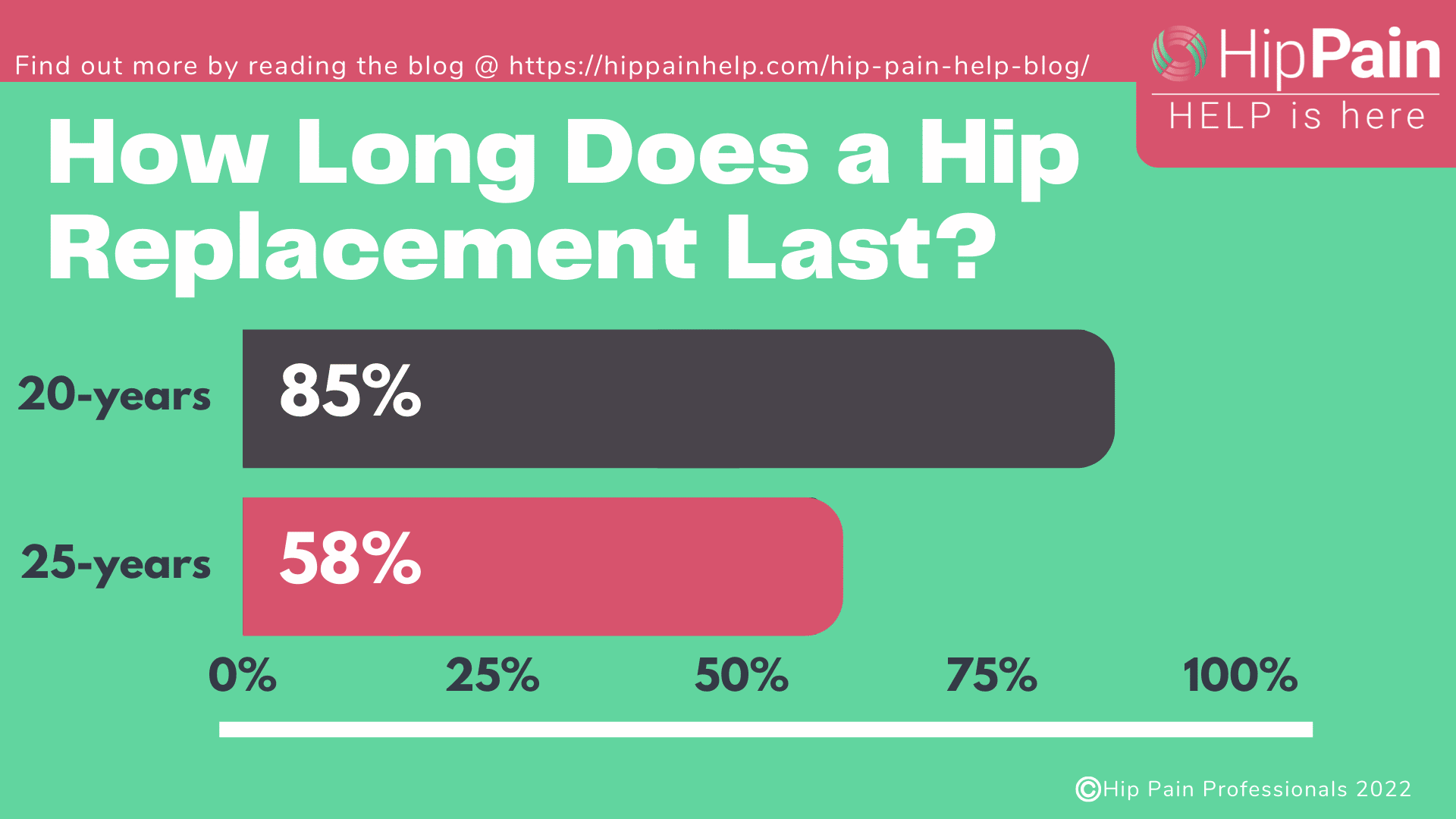
It’s important to note that the materials that were used when these surgeries were done, over 20 years ago, were much inferior to the materials used now. The newer materials are much more hard wearing, so surgeons are anticipating that the life of the prostheses they are using now could be much longer.
How long a hip prothesis is likely to last will be a factor in the surgical decision making, together with the age of the patient. Someone young who is likely to need their hip revised at some time in the future, may be considered a possible candidate for hip resurfacing.3
Who is suitable for Hip Resurfacing
Up until recently, hip resurfacing was considered as an option for the larger framed male who is less than 65 years of age, so the younger patient. However, the research is constantly evolving in this newer area of hip arthroplasty surgery, and resurfacing may be an option in some over 65 year old, older patients as long as they meet certain criteria.
Those who want to be more physically active after their replacement may also want to consider hip resurfacing as a surgical option.
Who is unsuitable for hip resurfacing
Generally, people with hip dysplasia are not suitable for hip resurfacing. People with hip dysplasia are more likely to struggle with hip arthritis but the shallow hip socket that is found in people with hip dysplasia means they are at higher risk of failure with this type of surgery.
As size of the bone at the top of the femur, the “femoral head size”, is currently extremely important in deciding if hip resurfacing is an option, females with hip arthritis are often not suitable for this type of surgery unless they meet the skeletal size requirements.
What are the different Approaches for Total Hip Replacement Surgery
There are usually one of three ways that your hip orthopaedic surgeon (“orthopedic surgeon” in the United States) will actually do your surgery, although other variations do exist. The most common approach is from the back of the hip, known as the posterior approach. Until recently the “anterior approach” was less frequently used, that is, approaching from the front of the hip. However, this is fast becoming a frequently offered alternative by many surgeons. The lateral approach is the third approach that has been around for some time.
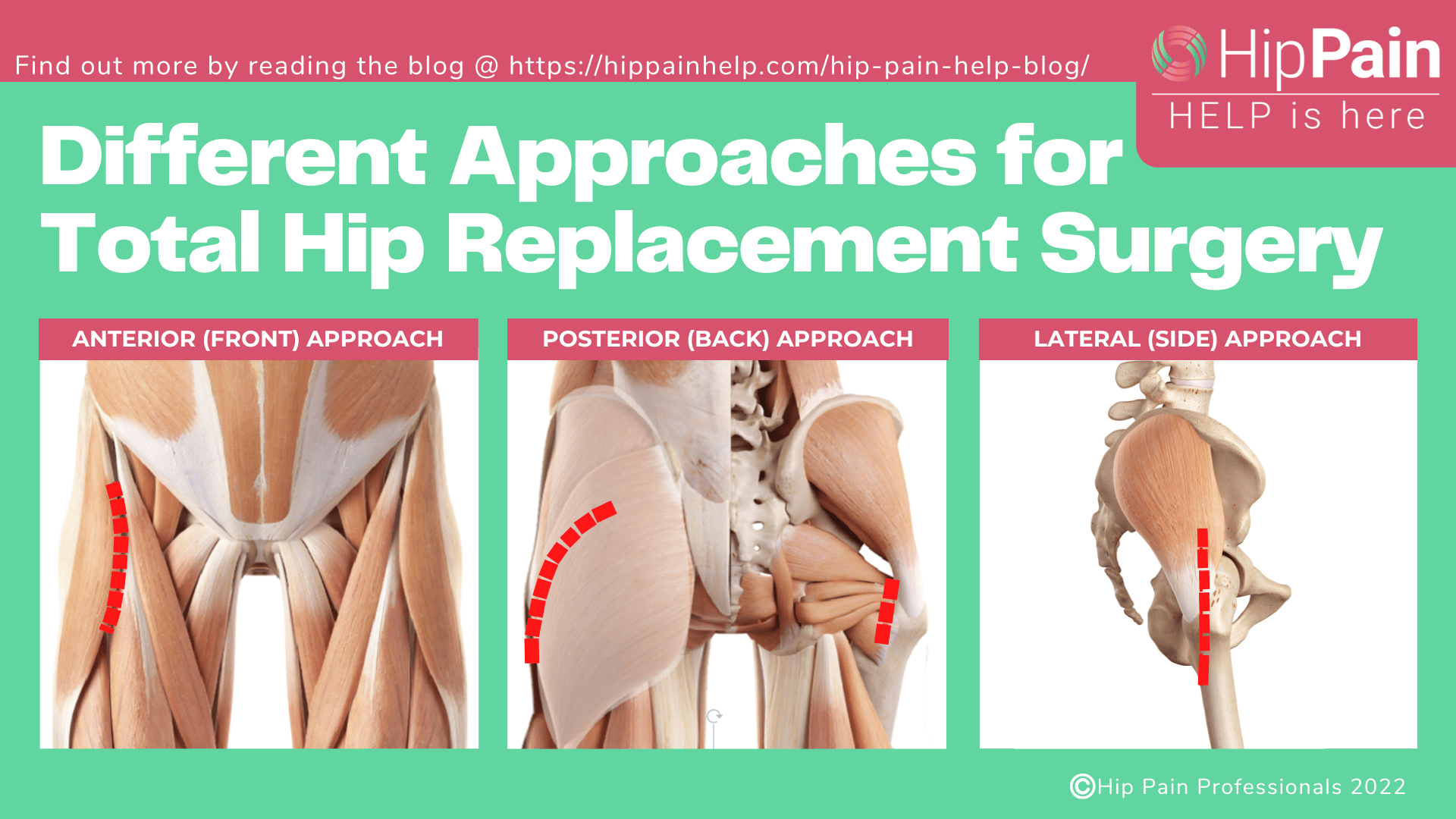
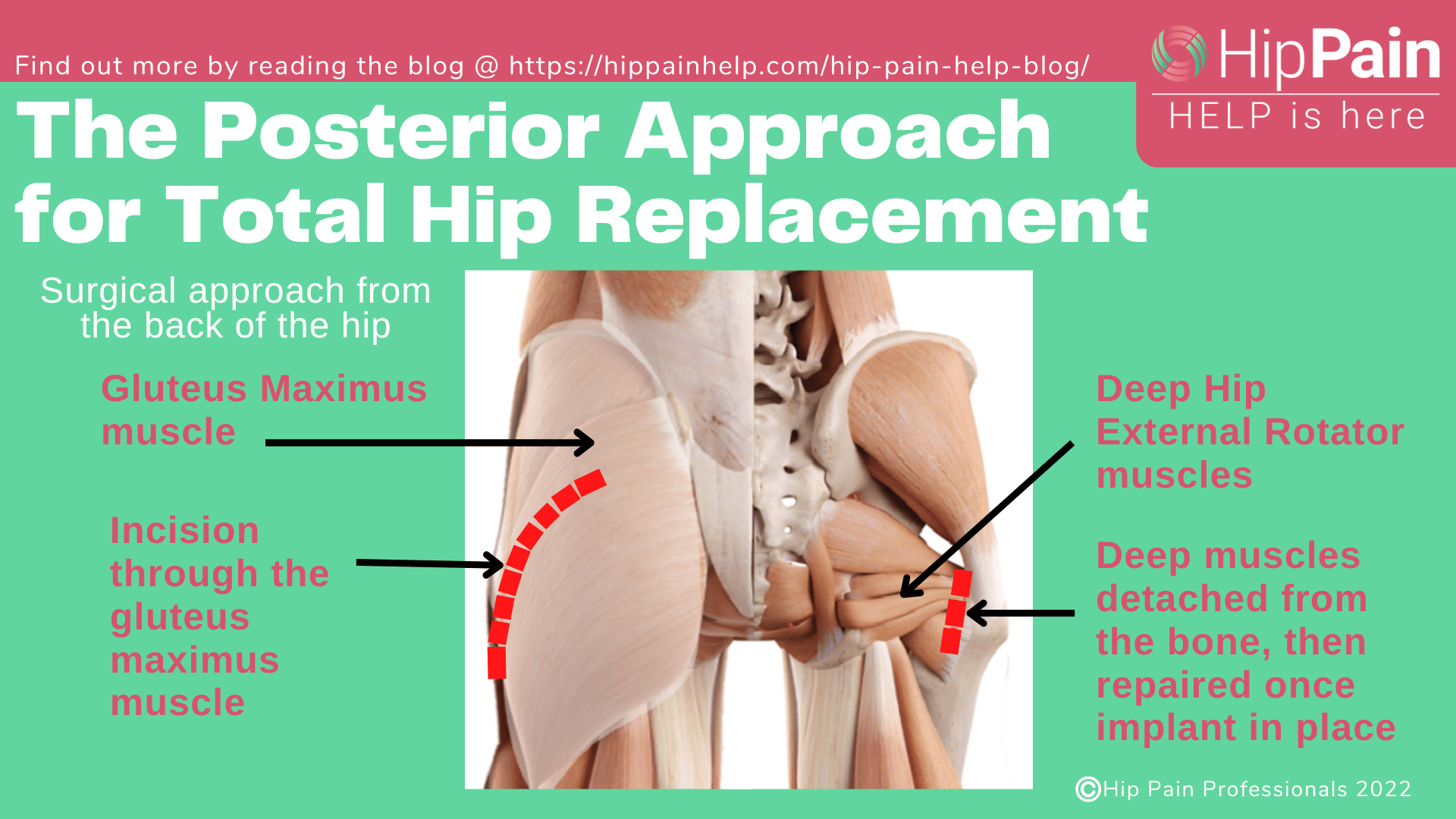
The posterior approach for total hip arthroplasty.
The surgeon will cut through the gluteus maximus muscle at the back of the hip and detach the deep hip external rotator muscles to view the back of the hip joint.
- This is the most commonly used approach.
- Offers the surgeon excellent access to the hip joint.
- The abductor muscles, or the muscles at the side of the hip are spared. This means patients are less likely to limp in the recovery period than those who have a lateral approach (see below).
- The sciatic nerve, a large and very important nerve in the back of the hip can be clearly seen, making it easier to protect this structure.
- The disadvantage of approaching from the back is that there can be a higher rate of dislocation after surgery, compared to other approaches. However, dislocation rates have been improving over time and some recent studies show rates as low as other surgical approaches. It is always important that post-operative instructions are followed to keep the hip safe in the healing period.
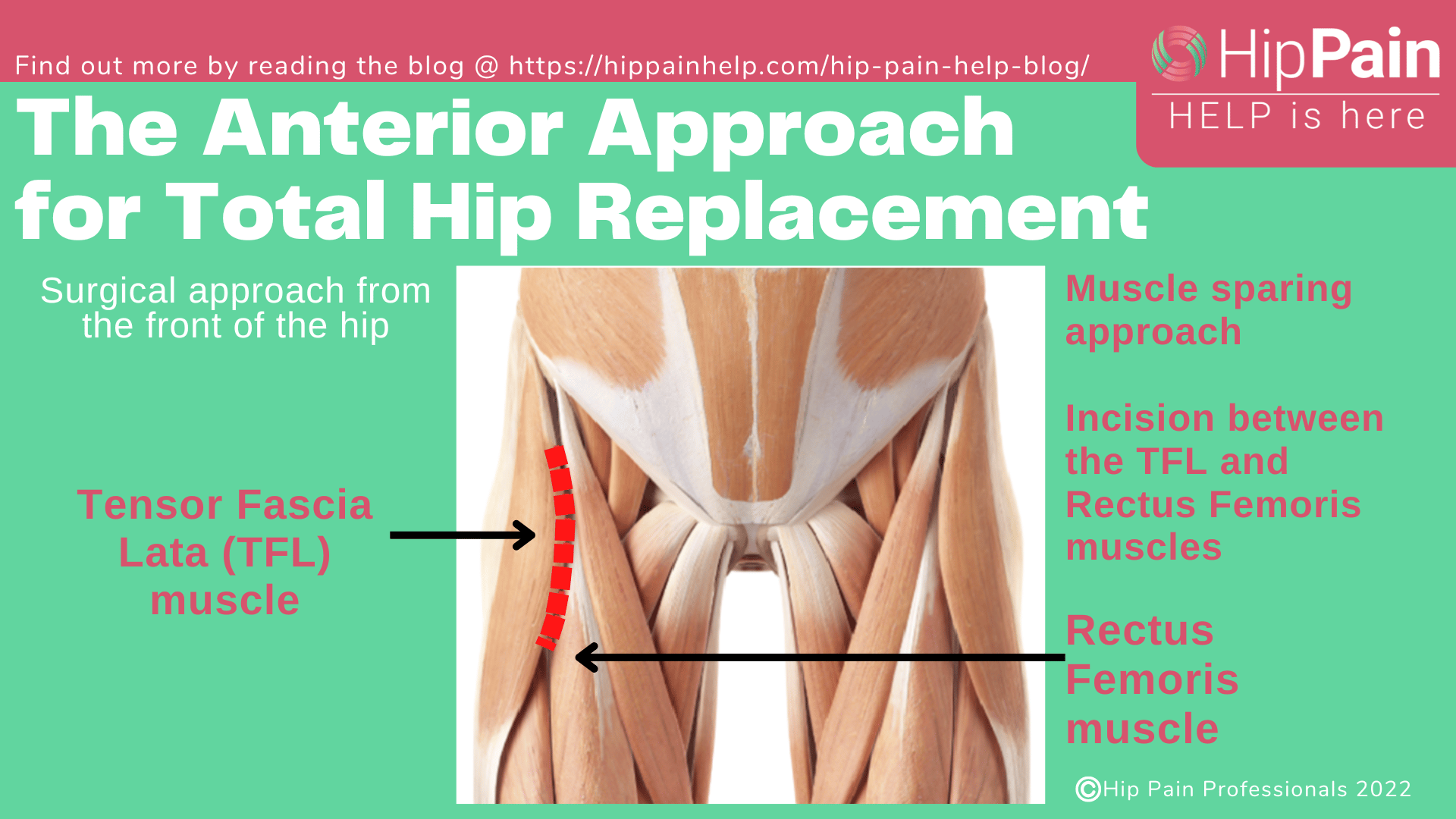
The anterior approach for total hip arthroplasty
The anterior approach, or anterior hip replacement, is where the surgeon approaches from the front of the joint. They go through between two of the major muscles at the front of the hip, the rectus femoris and the TFL.
- No muscles are cut and so no muscles need to be repaired afterwards.As the muscles at the side and back of the hip are not cut, there is less chance of dislocation afterwards so there are less restrictions with what you can and cannot do after your surgery compared with other approaches.
- Patients often require less time in hospital and can achieve a faster recovery in the early phases, although with improvement in surgical technique and physical therapy post operative routines all approaches generally do well in the long term.
- As the surgery is performed with the patient lying on their back, the position of the new hip prosthesis can be checked with xray during the hip surgical procedure.
- The surgeon has to work through a smaller “window” so this is not the typical choice for more complex cases or difficult revision surgery.
- This approach requires specific training and instruments that may not be available at some hospitals.