What is FAI or FAIS?
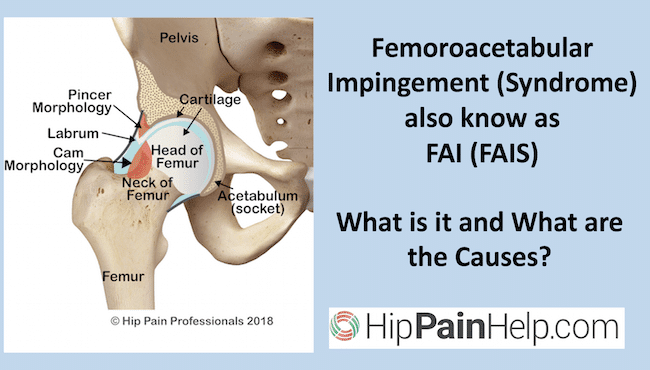
What are the causes of femoroacetabular impingement and what is it? You may have been diagnosed with femoroacetabular impingement, femoroacetabular impingement syndrome or hip impingement, or if you’ve seen more than one health professional, you may well have been given two different diagnoses. Or maybe you’ve just been searching the internet to make your own diagnosis and are confused about the different terminology. Let’s explore the different diagnoses and causes of FAIS.
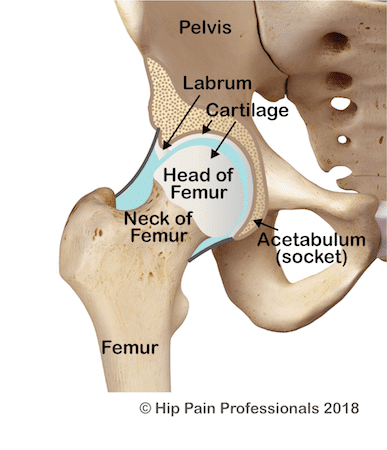
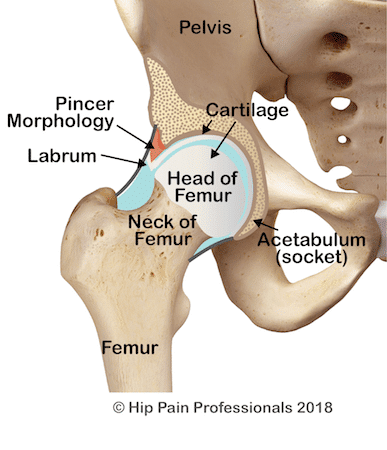
Figure 1: Basic Anatomy of the Hip as Viewed From the Front
Femoroacetabular impingement (FAI) refers to early contact (impingement) between the bones of the hip during movement, due to a variation in shape of the bones of the hip joint (femur (thigh bone) and/or acetabulum (hip socket)). This may result in reduced range of motion (stiffness) and, in a relatively small percentage of people, hip pain associated with extra forces being placed across joint structures such as the acetabular labrum and cartilage (Figure 1).
What is Femoroacetabular Impingement Syndrome (FAIS)?
Painful FAI is referred to as Femoroacetabular Impingement Syndrome (FAIS). A published consensus of world experts¹ agreed that the diagnosis of FAIS requires 3 key features:
- FAI bony variations observable on XRay or MRI Scans
- Hip or groin pain related to particular motions or positions
- Pain and restricted range of motion on clinical tests performed by a health professional
Types Of FAI: Bone Changes that are Attributed to The Causes of FAI
3 different bony shape configurations may be associated with and result in the cuases of FAI.
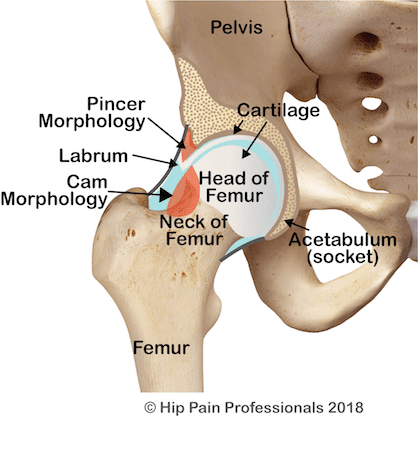
1. Cam Morphology (shape) – Cam FAI
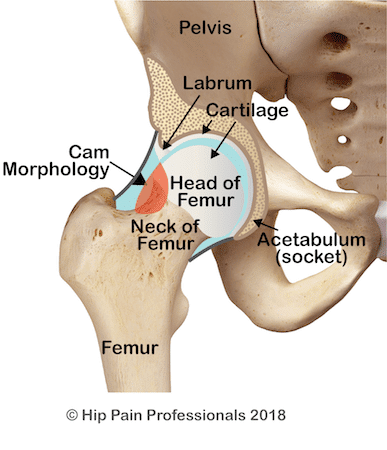
Cam morphology or cam-type morphology (Figure 2) is where the femoral head is non-spherical and the junction between the head and neck of the femur is thicker than normal. This thickening means that as the hip moves into flexion (knee to chest) or internal rotation (knee turns in) there is less bony clearance between the head/neck junction and the acetabulum. When the cam area comes into contact with the acetabulum, it is referred to as Cam Impingement or Cam FAI. This may result in restricted range of motion and higher loads than normal being placed on the labrum and the cartilage on the outer edge of the acetabulum.
2. Pincer Morphology (shape) – Pincer FAI
Pincer morphology or pincer-type morphology (Figure 3) refers to a variation in shape or orientation of the acetabulum. of the whole femoral head by the acetabulum may occur when the socket is deeper than average (global overcoverage) or the edge of the socket may sit lower at the front of the femoral head due to an orientation where the socket faces a little more backwards than normal (acetabular retroversion – focal overcoverage). Both situations may result in restricted movement as the femur and the acetabulum come together earlier in range, referred to as Pincer Impingement or Pincer FAI. The labrum can again be put under higher stress.
3. Cam & Pincer Morphology – Mixed FAI
A mix of cam and pincer shapes (Figure 4) can also occur, referred to as Mixed FAI.
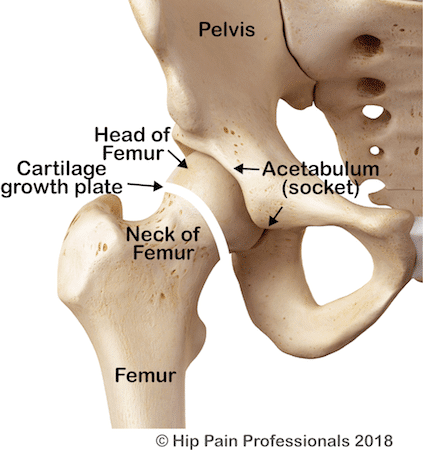
What are the Causes of FAI?
FAI is a condition related to alterations in the pattern of bony growth4. Bones continue to grow and change shape during childhood and adolescence. Growing bones have cartilaginous growth-plates or epiphyses from which the bone grows and extends, before fusing into hard bone as early adulthood is reached. The growth plates (Figure 5) are influenced by the amount and type of physical loads they are exposed to. The most common type of FAI, Cam FAI, is thought to develop in response to physical activity that places load across the growth plate in the neck of the femur. High load across the growth plate may stimulate excess bone to be laid down in this area.
Researchers have identified a number of possible factors that may contribute to this bony response and risk of developing a ‘cam-type’ bony shape:
- High exposure to twisting and bending forces across the femoral neck
- Involvement in sports that involve these types of forces – Soccer/football codes, hockey, basketball4
- Training 4 or more times/week
- Being male – a cam shape is much more common in males

Change in the shape of the head and/or neck of the femur can also be related to childhood conditions such as Legg-Calve Perthes Disease or Slipped Capital Femoral Epiphysis.
How Can A Hip Pain Professional Help?
An interview and physical assessment with a Hip Pain Professional can help clarify which factors may have contributed to the development of your hip pain. A specific, personalised plan can then be actioned to help you overcome your problem.
References
- Griffin, D., Dickenson, E., O’Donnell, J et al. (2016). The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. British Journal of Sports Medicine, 50(19), pp.1169-1176.
- Reiman, M. and Thorborg, K. (2015). Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? British Journal of Sports Medicine, 49(12), pp.782-784.
- Frank, J., Harris, J., Erickson, B., Slikker, W., Bush-Joseph, C., Salata, M. and Nho, S. (2015). Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 31(6), pp.1199-1204.
- Zadpoor, A. (2015). Etiology of Femoroacetabular Impingement in Athletes: A Review of Recent Findings. Sports Medicine, 45(8), pp.1097-1106.
- Griffin, D., Dickensen, E., Hobson, R., et al. (2018). Hip arthroscopy compared to best conservative care for the treatment of femoroacetabular impingement syndrome: a randomised controlled trial (UK FASHIoN). Osteoarthritis and Cartilage, 26, pp.S24-S25.
- Mansell, NS., Rhon, DI., Meyer, J., Slevin, JM., Marchant, BG. (2018). Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: A randomized controlled trial with 2-year follow-up. American Journal of Sports Medicine, 46(6), pp.1306-1314.
- Thorborg, K., Kraemer, O., Madsen, AD., Holmich, P. (2018). Patient-reported outcomes within the first year after hip arthroscopy and rehabilitation for femoroacetabular impingement and/or labral injury: The difference between getting better and getting back to normal. American Journal of Sports Medicine, 46(11), pp.2607-2614.
- Freke, MD., Kemp, J., Svege, I., Risberg, MA., Semciw, A., Crossley, KM. (2016). Physical impairments in symptomatic femoroacetabular impingement: a systematic review of the evidence. British Journal of Sports Medicine 2016, 50(19), pp.1180.